Gastroesophageal Reflux Disease (GERD)
Acid reflux, also known as heartburn, happens to almost everyone. But when it continues for many weeks and occurs several times a week, you may have gastroesophageal reflux disease – GERD.
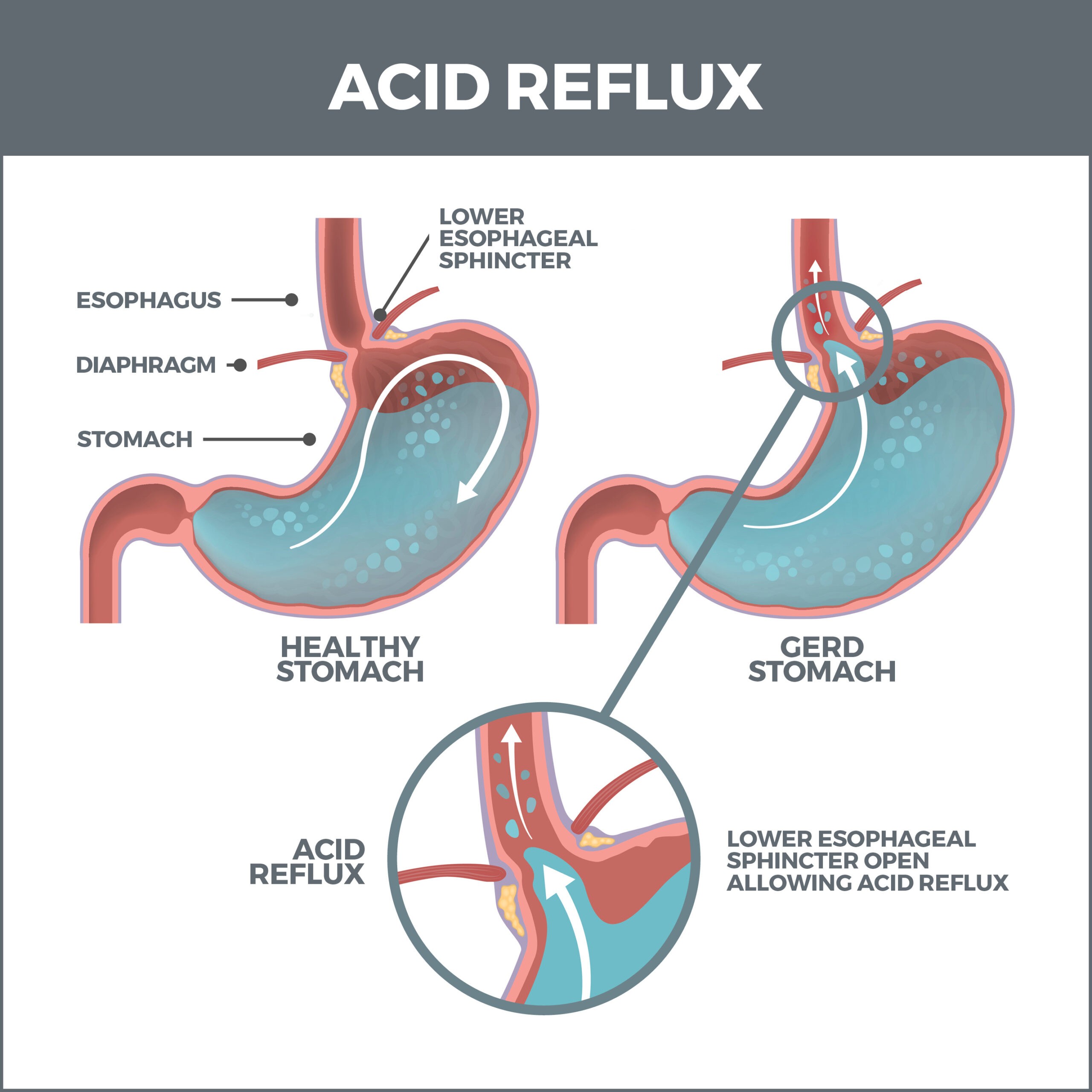
GERD is a severe digestive disorder caused by stomach acid backing up into your esophagus. This condition happens when the valve between your esophagus and your stomach (the lower esophageal sphincter or LES) weakens or relaxes when it shouldn’t.
When the LES operates properly, it opens so food can enter the stomach and closes to prevent food and digestive juices from backwashing into the food pipe. When it malfunctions, the persistent acid can damage tissue and lead to other serious conditions.
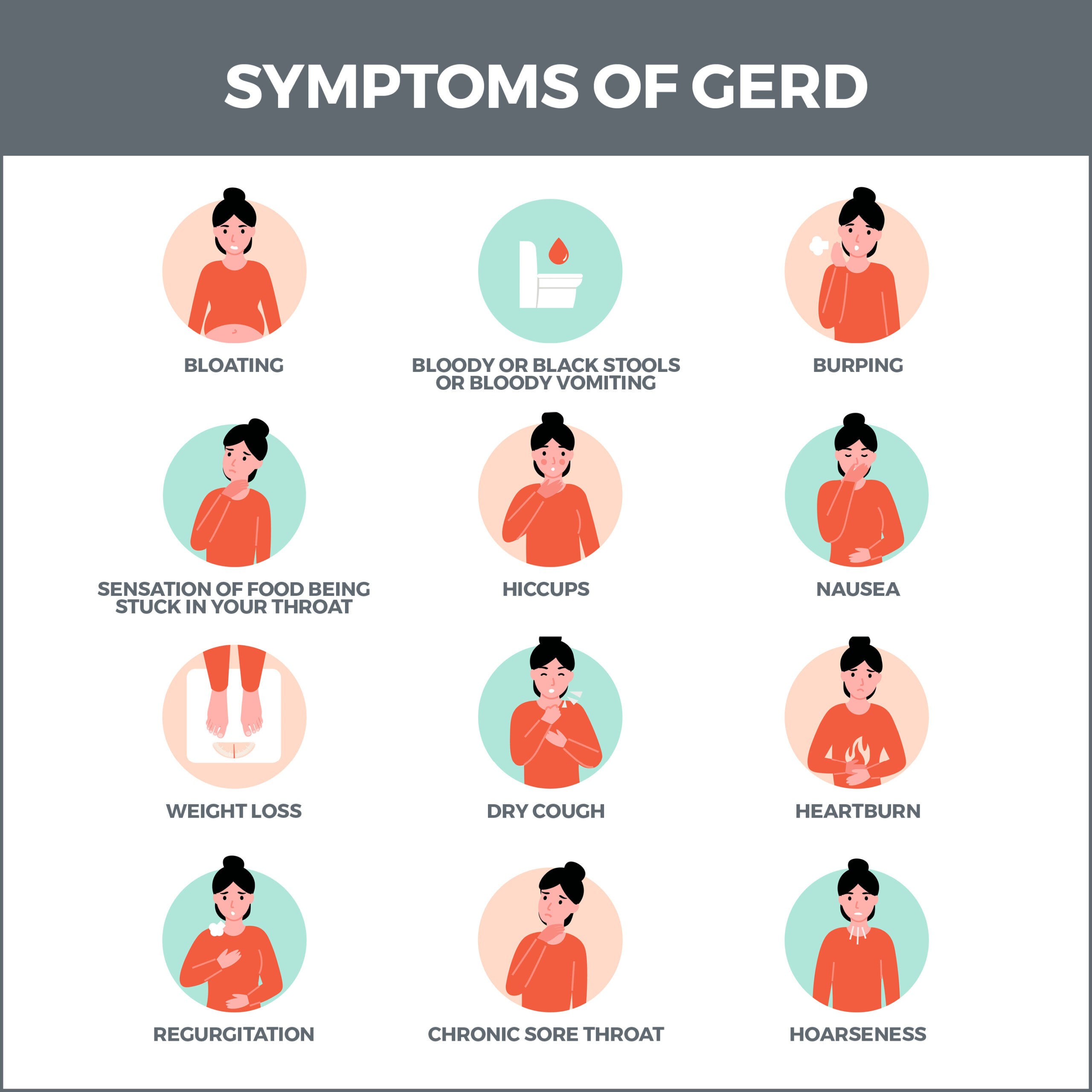
GERD’s primary symptom is acid reflux, which causes heartburn, a burning sensation in your chest or throat. Other symptoms may include:
Regurgitation of liquid or food into your mouth.
- Difficulty swallowing.
- Painful swallowing.
- Hoarse voice.
- Bad breath.
- Nausea.
- Chest pain.
- Feeling that there is a lump in your throat.
If you suffer from nighttime GERD, you might also experience:
- Disrupted sleep.
- New or worsening asthma.
- Chronic cough.
- Laryngitis.
What Causes GERD?
Being overweight is the most significant cause of GERD, but many other conditions can be responsible for it, including:
- Hiatal Hernia – A hiatal hernia develops when your stomach abnormally bulges into your chest through an opening in your diaphragm (a thin muscle between the chest cavity and abdomen). A hiatal hernia blocks normal food intake, causing GERD symptoms such as heartburn, acid reflux, and difficulty swallowing. Hiatal hernias typically affect people 50 and older.
- Asthma – When digestive juices continuously damage the esophagus and the passageway to the lungs, it can interfere with breathing. The backflow of stomach acid can also cause airways to protectively constrict, making breathing difficult. Lastly, this acid can make the lungs more sensitive to pollen, dust, and other airborne contaminants, creating shortness of breath.
- Anxiety – People suffering from GERD may develop anxiety because they fear the discomfort and pain it causes. Additionally, a person’s stress levels can intensify GERD.
- Rheumatoid Arthritis – Rheumatoid arthritis (RA) is an autoimmune disorder that targets the body’s joints. The same inflammation that attacks your joints can also impact your digestive tract.
- Gastroparesis (delayed emptying of the stomach) – Gastroparesis is the paralysis of the digestive system. When food lingers in the stomach and cannot leave the stomach properly, it can cause GERD.
- Lupus – Lupus is a long-term autoimmune condition that attacks your tissues and organs. When it inflames the esophagus, it can cause stomach acids to back up into the throat.
- Excessive Pressure on the Abdomen – Pregnant women are susceptible to GERD. The condition is also linked to increased abdominal pressure from obesity, coughing, straining to pass a bowel movement, or lifting a heavy object.
- Medications – Medications that can cause GERD include antidepressants, NSAIDs, iron supplements, antibiotics, and drugs for high blood pressure.
Certain foods are more likely to trigger GERD than others. These include:
- Fatty foods.
- Fried foods.
- Fast food.
- Onions.
- Tomatoes and tomato sauce.
- Coffee.
- Alcohol.
- Soda and energy drinks.
Simple lifestyle changes can relieve GERD. These include:
- Quitting smoking.
- Maintaining a healthy weight.
- Avoiding heavy evening meals.
- Thoroughly chewing your food.
- Eating slowly.
- Waiting several hours after eating before lying down or going to bed.
- Elevating your head six to eight inches at bedtime.
How is GERD Diagnosed?
If your gastroenterologist suspects that you have GERD, they may order these tests:
- Ambulatory 24-hour pH Probe – Considered the “gold standard” of GERD diagnostic tests, this procedure involves passing a small tube with a pH sensor through the nose to the esophagus. It is worn for 24 hours and determines how severely the esophagus is harmed by acid.
- Esophogram – During an esophogram, you’ll drink barium sulfate. This metallic substance gives more definition to parts of the body that are being x-rayed.
- Upper GI Series – This test uses special x-rays that show your esophagus, stomach, and the upper part of your small intestine.
- Upper Endoscopy – A flexible tube with a tiny camera is passed into your esophagus to analyze and collect a tissue sample.
- Esophageal Manometry and Impedance Study – This procedure determines the strength of the muscles in your esophagus and whether your esophageal muscles improperly contract.
What is GERD in children?
Distinguishing between normal, physiologic reflux and GERD in children is important. Most infants with GER are happy and healthy even if they frequently spit up or vomit, and babies usually outgrow GER by their first birthday. Reflux that continues past one year of age may be GERD. Studies show that GERD is common and may be overlooked in infants and children. For example, GERD can present as repeated regurgitation, nausea, heartburn, coughing, laryngitis, or respiratory problems like wheezing, asthma, or pneumonia. Infants and young children may demonstrate irritability or arching of the back, often during or immediately after feedings. Infants with GERD may refuse to feed and experience poor growth.
Talk with your child’s doctor if reflux-related symptoms occur regularly and cause your child discomfort. Your doctor may recommend simple strategies for avoiding reflux, such as burping the infant several times during feeding or keeping the infant in an upright position for 30 minutes after feeding. If your child is older, your doctor may recommend that your child eat small, frequent meals and avoid the following foods:
- Sodas that contain caffeine.
- Chocolate.
- Peppermint.
- Spicy foods.
- Acidic foods like oranges, tomatoes, and pizza.
- Fried and fatty foods.
Avoiding food 2 to 3 hours before bed may also help. Your doctor may recommend raising the head of your child’s bed with wood blocks secured under the bedposts. Just using extra pillows will not help. If these changes do not work, your doctor may prescribe medicine for your child. In rare cases, a child may need surgery. For information about GER in infants, children, and adolescents, see the Gastroesophageal Reflux in Infants and Gastroesophageal Reflux in Children and Adolescents fact sheets from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Points to Remember
- Frequent heartburn, also called acid indigestion, is the most common symptom of GERD in adults. Anyone experiencing heartburn twice a week or more may have GERD.
- You can have GERD without having heartburn. Your symptoms could include a dry cough, asthma symptoms, or trouble swallowing.
- If you have been using antacids for more than two weeks, it is time to see your gastroenterologist. They can treat GERD.
- Lifestyle and dietary changes can help relieve the symptoms of GERD. Many people with GERD also need medication. Surgery may be considered as a treatment option.
- Most infants with GER are healthy even though they may frequently spit up or vomit. Most infants outgrow GER by their first birthday. Reflux that continues past one year of age may be GERD.
- The persistence of GER, along with other symptoms – arching and irritability in infants or abdominal and chest pain in older children – is GERD. GERD is the outcome of frequent and persistent GER in infants and children and may cause repeated vomiting, coughing, and respiratory problems.
GERD Treatment Options
These are over-the-counter medications that address GERD symptoms:
- Antacids.
- Foaming agents
- H2 Receptor Blockers (histamine blockers).
- Proton Pump Inhibitors.
- Prokinetics
Antacids, which are medications that neutralize stomach acid, are the first line of defense against GERD. Examples of these include Maalox®, Pepto-Bismol®, and Rolaids®. If your symptoms persist or worsen, stronger treatments may be necessary.
Foaming agents such as Gaviscon® work by covering your stomach contents with foam to prevent reflux.
H2 receptor blockers are medications that neutralize the acid already in your stomach and decrease acid production. Examples include such as Tagamet HB® (cimetidine), Pepcid AC® (famotidine), Axid AR® (nizatidine), and Zantac 75® (ranitidine).
Protein pump inhibitors prevent acid from being released into the stomach. These medications must be taken 30 to 60 minutes before eating. Examples of these include Prilosec® (omeprazole), Prevacid® (lansoprazole), and Nexium® (esomeprazole), which are available by prescription. Some are also available in over-the-counter strength. Proton pump inhibitors are more effective than H2 blockers and can relieve symptoms and heal the esophageal lining in almost everyone with GERD.
Prokinetics help strengthen the lower esophageal sphincter (LES) and make the stomach empty faster. This group includes Urecholine® (bethanechol) and Reglan® (metoclopramide). Metoclopramide also improves muscle action in the digestive tract. Prokinetics have frequent side effects that limit their usefulness – fatigue, sleepiness, depression, anxiety, and problems with physical movement.
Because drugs work in different ways, combinations of medications may help control symptoms. People who get heartburn after eating may take both antacids and H2 blockers. The antacids work first to neutralize the acid in the stomach, and then the H2 blockers act on acid production. By the time the antacid stops working, the H2 blocker will have stopped acid production. Your gastroenterologist is the best source of information about how to use medications for GERD.
Complications of GERD
Untreated, chronic GERD can cause serious complications. Inflammation of the esophagus from refluxed stomach acid can damage the lining and cause bleeding or ulcers – also called esophagitis. Scars from tissue damage can lead to strictures – narrowing of the esophagus – that make swallowing difficult. Some people develop Barrett’s esophagus, in which cells in the esophageal lining take on an abnormal shape and color. Over time, the cells can lead to esophageal cancer, which is often fatal. Persons with GERD and its complications should be monitored closely by a physician.
Studies have shown that GERD may worsen or contribute to asthma, chronic cough, and pulmonary fibrosis.
Surgery
In cases of severe GERD, if all other treatment options have been unsuccessful, surgery may be necessary. Types of these procedures include:
- Fundoplication – This surgery involves wrapping the fundus (the upper curve of the stomach) around the esophagus and sewing it into place. This strengthens the lower esophageal sphincter (LES), preventing stomach acid from backing up into the esophagus. If you also have a hiatal hernia, it can be corrected during fundoplication.
- Transoral Incisionless Fundoplication (TIF) – Less invasive than fundoplication, this surgery uses an endoscope (a thin tube with a light attached) to wrap the stomach around the LES and fasten it with plastic closures.
- LINX Surgery – A tiny band of magnetic titanium beads surrounds and squeezes the LES during this procedure. The magnet pulls the beads together, closing off the esophagus from the stomach. When you swallow, the beads loosen to permit food to enter the stomach, then close to prevent acid from traveling up the esophagus.
- Stretta Procedure – A Stretta procedure involves sending an endoscope down your throat to the lower esophageal sphincter (LES) and upper stomach. Next, radiofrequency energy heats the muscles, causing them to thicken and form a stronger barrier against stomach acid.
Contact Us
Are you suffering from gastroesophageal reflux disease – GERD? Contact us today. The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority.



