
Crohn’s Disease
Crohn’s disease is an inflammatory bowel disease (IBD) that can affect any part of the digestive tract from the mouth to the anus. It typically strikes the colon and small intestine and can range from minor aches to crippling pain. Crohn’s disease is a lifelong, incurable condition, but its symptoms can be managed so that you can live an active lifestyle.
Crohn’s disease is often confused with IBS (irritable bowel syndrome) because they have similar names and symptoms, but they are two different conditions.
IBS is a disorder of the digestive tract’s function (how it works), while IBD, or Crohn’s disease, is a disorder of its structure (chronic inflammation caused by an overactive immune response).
What Causes Crohn’s Disease?
Normally, your immune system recognizes foreign invaders and attacks them. This protects your digestive tract.
If you have Crohn’s disease, your immune system misinterprets food and other harmless substances as threats and releases white blood cells that attack the bowels’ lining. This triggers ulceration, thickening of the intestinal wall, and chronic inflammation. Crohn’s disease can affect the whole bowel wall or occur in patches.
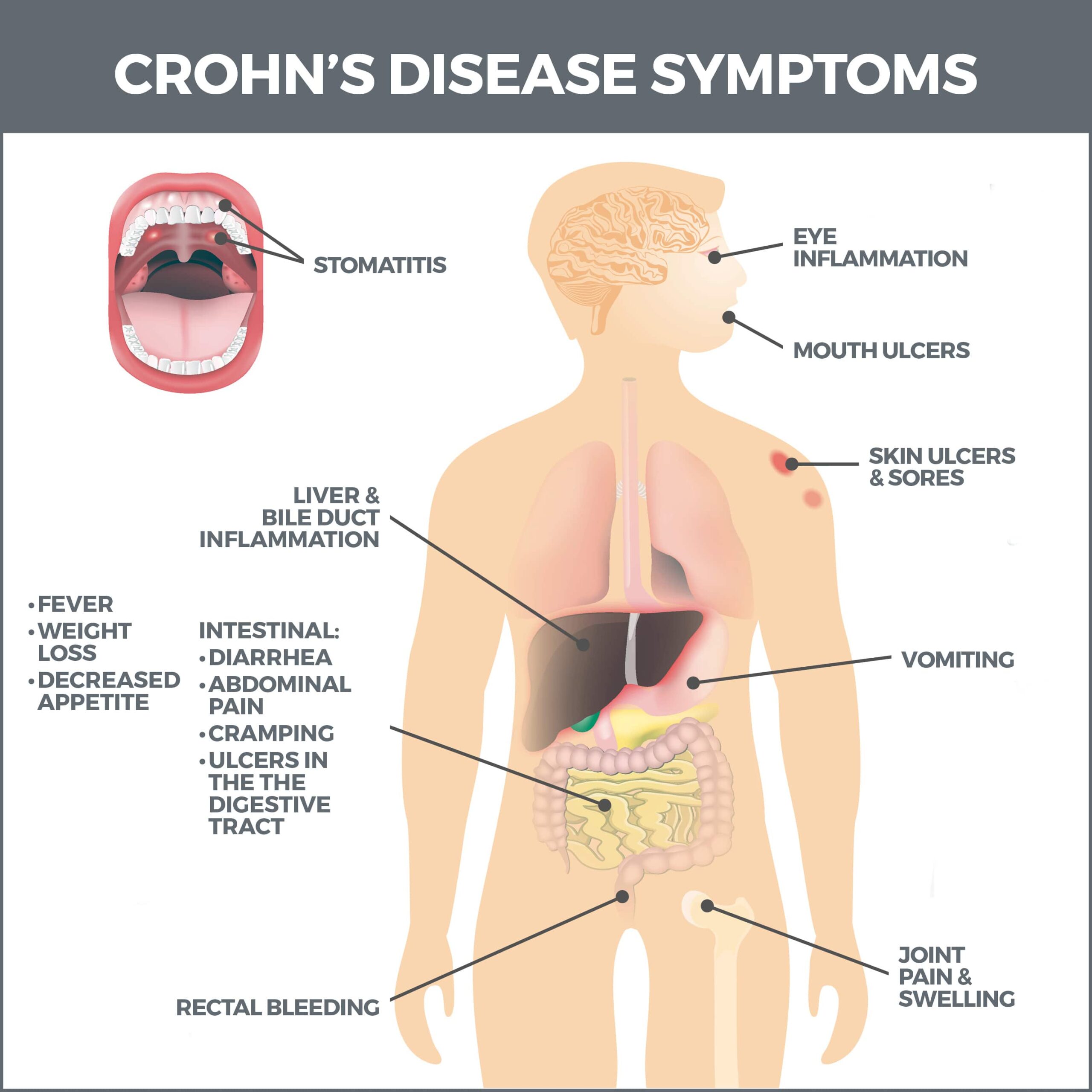
What are Crohn’s Symptoms?
Crohn’s symptoms usually develop gradually and can worsen over time. The condition usually has periods of remission alternating with periods of flare-ups. Flare-ups can last weeks or months and can occur after months or even years of remission.
Early symptoms include:
- Chronic diarrhea (the most common symptom).
- Abdominal cramps.
- Frequent need to have a bowel movement.
- Feeling as though your bowels aren’t entirely empty after you’ve gone to the bathroom.
- Bloody stool.
- Loss of appetite.
- Fever.
- Belly pain and cramping.
- Yeast infections that invade the intestinal tract and lungs.
Severe Crohn’s disease may cause:
- Liver or bile duct inflammation.
- Skin or joint inflammation.
- Anemia (iron deficiency).
- Kidney stones.
- Anal drainage and pain.
- Ulcers that form anywhere from the mouth to the anus.
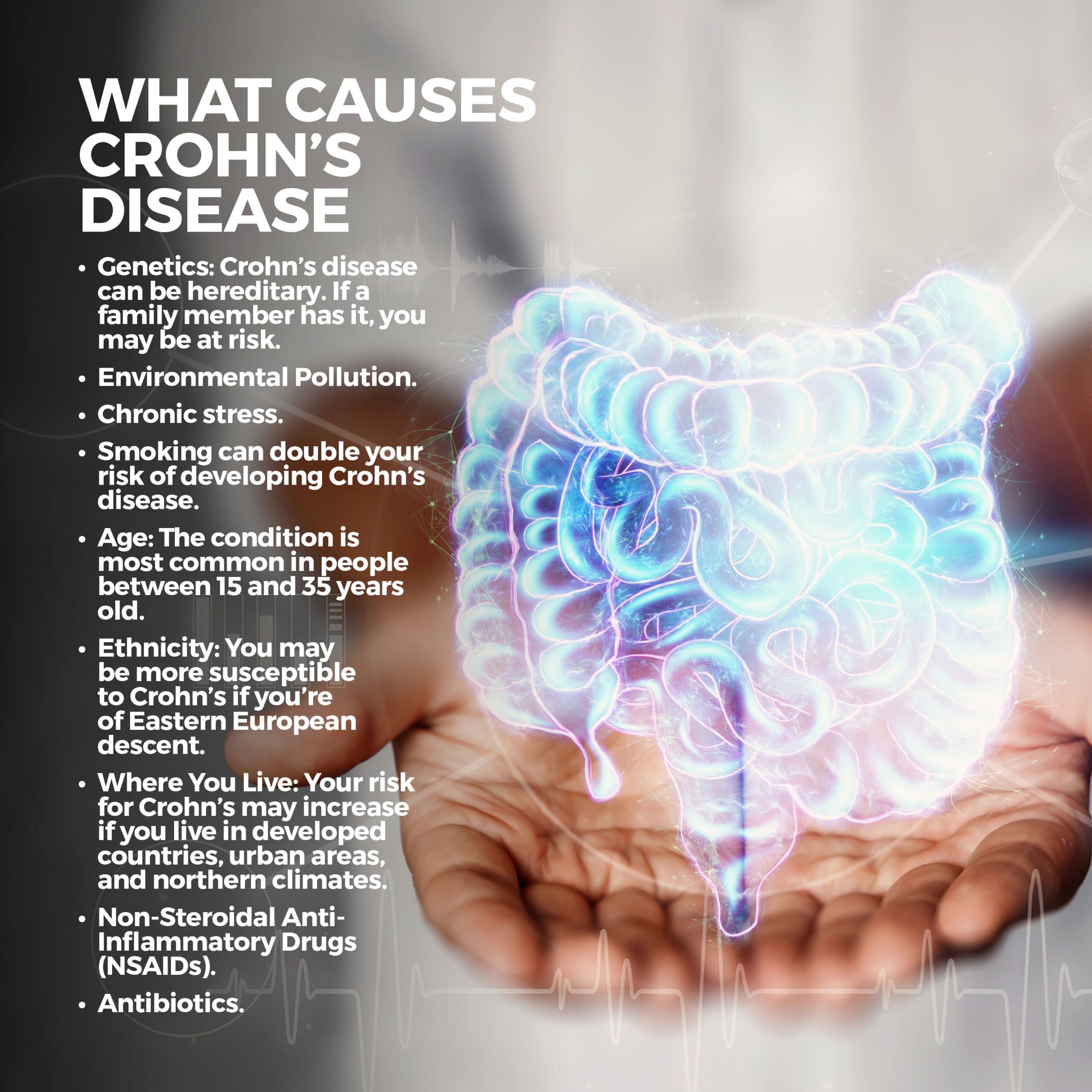
What Causes Crohn’s Disease?
Although scientists are still studying the causes of the condition, there is evidence it may be triggered by:
- Genetics: Crohn’s disease can be hereditary. If a family member has it, you may be at risk.
- Environmental pollution.
- Chronic stress.
- Smoking: Smoking can double your risk of developing Crohn’s disease.
- Age: The condition is most common in people between 15 and 35 years old.
- Ethnicity: You may be more susceptible to Crohn’s if you’re of Eastern European descent.
- Where you live: Your risk for Crohn’s may increase if you live in developed countries, urban areas, and northern climates.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs).
- Antibiotics.
What Are the Different Types of Crohn’s Disease?
There are four types of Crohn’s disease. Each impacts a different part of your digestive tract:
- Ileocolitis: Ileocolitis is the most common form of Crohn’s and affects the small intestine and part of the large intestine.
- Jejunoileitis: This type of Crohn’s disease causes patches of inflammation in the small intestine’s upper half (the jejunum).
- Ileitis: Ileitis causes swelling and inflammation in the small intestine (the ileum).
- Gastroduodenal: Gastroduodenal Crohn’s inflames the top of the small intestine (the duodenum) and stomach.
How is Crohn’s Disease Diagnosed?
Since the disease’s symptoms may mimic other conditions, your physician will do tests to rule them out and make an accurate Crohn’s diagnosis. These tests include:
- Stool Test: During this test, part of your stool will be examined for bacteria or parasites.
- Blood Test: A blood test can reveal high amounts of white cells indicative of an infection or inflammation. It also identifies low red blood cell counts (anemia). One in three people who have Crohn’s disease has anemia.
- Computed Tomography (CT) Scan: A CT scan produces 3-D “cross-section” images of your digestive tract. It permits your doctor to see the extent of inflammation more distinctly.
- Colonoscopy: A colonoscopy is a procedure that is performed to examine your large intestine. Using a flexible tube with a light and camera, your doctor can analyze your rectum and colon for abnormalities and collect a tissue sample, if needed.
- Upper Gastrointestinal Exam: When having this procedure, you’ll swallow a liquid called barium sulfate, making the upper part of your digestive tract show up more clearly on x-rays.
- Upper Gastrointestinal Endoscopy: During an upper gastrointestinal endoscopy, your doctor passes a tube with an attached camera through your mouth and into your throat. The camera will reveal irregularities, and tissue samples can also be collected.
Treatment
There is no cure for Crohn’s disease. But some treatments can suppress inflammation and promote remission. The longer inflammation is suppressed, the more time your intestines have to heal.
Medications are usually the first line of defense against the condition. These include:
- Aminosalicylates: Aminosalicylates target digestive tract inflammation. These are effective for mild Crohn’s symptoms.
- Biologics: Biologics are medications made from living cells. Vaccines, for instance, are biologics. They home in on intestinal proteins that cause inflammation. Biologics are delivered via an IV. After the first dose, you’ll typically receive a dose at two weeks, four weeks, and then every eight weeks after.
- Corticosteroids: Corticosteroids are used for moderate to serious Crohn’s. They reduce swelling and soothe your immune system. They can cause dangerous side effects, so they’re not prescribed long-term.
- Immunomodulators: These drugs stop inflammation by altering your immune system. They’re usually the last resort when other medications have failed. One drawback is that it may be weeks or months before they start working.
In severe cases of Crohn’s, surgery may be necessary. An estimated 75 percent of people who have Crohn’s will eventually need surgery. These procedures include:
- Bowel Resection: Damaged segments of the intestine are removed, and the healthy parts are connected.
- Strictureplasty: Long-term inflammation can cause your intestine to thicken into scar tissue (strictures). Strictures can completely block food from traveling through your digestive tract. A strictureplasty expands this blockage so that food can pass through.
- Fistula Removal: A fistula is a tube-like opening that forms when an ulcer extends through the intestinal wall and abnormally connects organs that don’t typically connect. A fistula doesn’t heal on its own and must be surgically removed.
- Proctocolectomy/Colectomy: During these procedures, your colon, rectum, or both are removed.
Contact Us
Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority!



