Cirrhosis
Cirrhosis is an irreversible condition that permanently damages your liver and can lead to liver failure. Severe scarring and hardening, caused by a long-term assault of toxins, gradually destroys the organ’s ability to function correctly. This damage can’t be repaired, but further injury can be prevented if cirrhosis is caught early enough.
What is the Liver?
The liver is the largest organ in your body and is located on the right side of your abdomen. Parts of the intestines and pancreas are tucked under the liver. The liver has more than 500 functions. Some of the most important ones include:
- Removing chemicals, bacteria, and other impurities.
- Breaking down medications so they are easier for the body to use.
- Storing iron, copper, and vitamins A, D, E, K, and B12.
- Regulating amino acid production.
- Producing proteins for blood plasma.
- Producing bile, a substance that removes waste from the blood and breaks down fats.
- Converting excess glucose (sugar) into glycogen for storage and later retrieval for energy.
- Regulating blood clotting.
- Processing hemoglobin (a protein in red blood cells that allows blood to carry oxygen to your tissues).
When these functions are repeatedly interrupted, it can result in cirrhosis.
What is Cirrhosis?
When you have cirrhosis, your liver becomes so scarred that it can’t function normally. Whenever the organ is damaged, it tries to protect itself by forming scar tissue. This scar tissue builds up and replaces normal, healthy tissue. It also blocks your liver’s blood flow. As this condition worsens, your liver will begin failing.
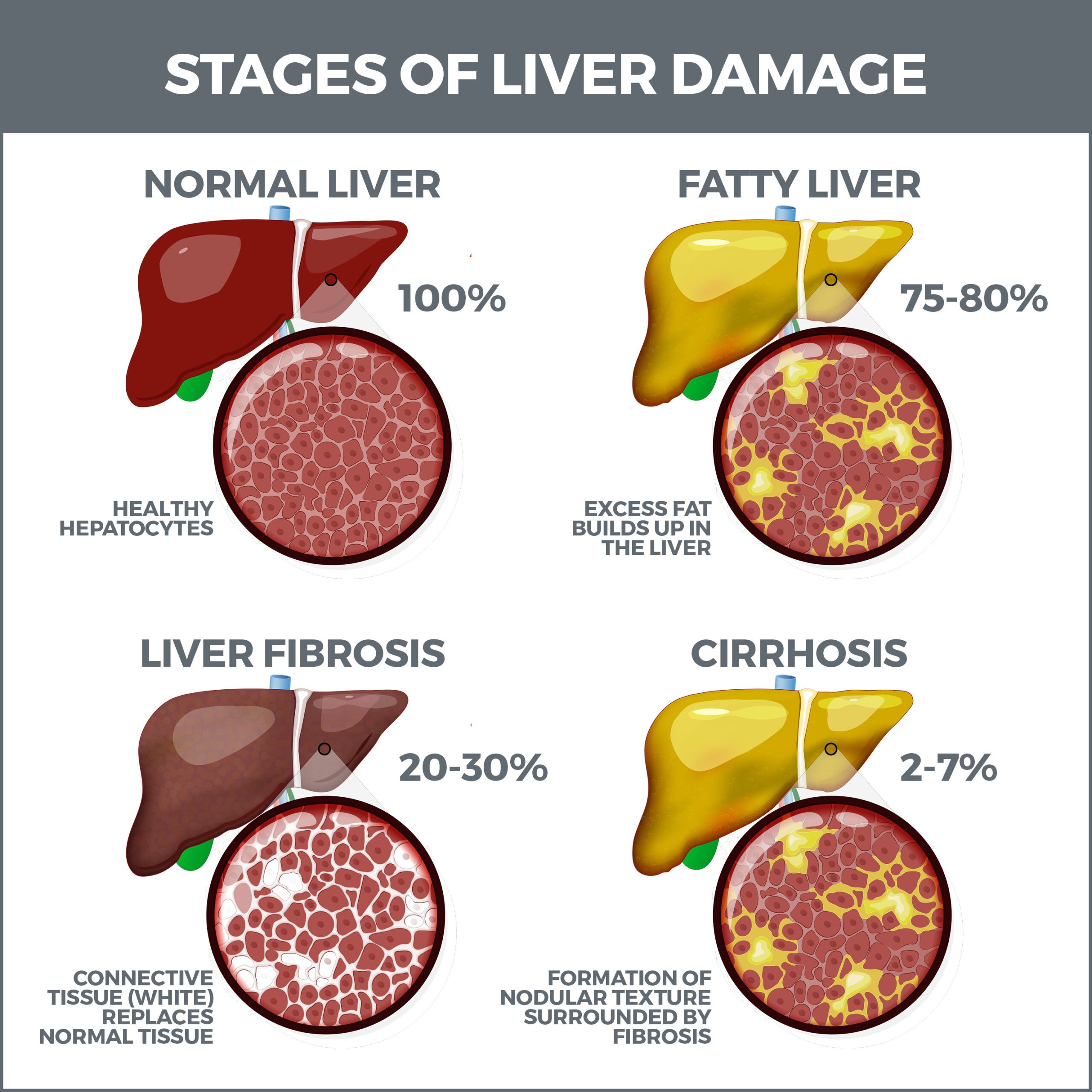
Cirrhosis is irreversible, but it may be prevented from worsening if it’s detected early. There are several phases of liver disease:
- Inflammation – In the early phases of liver disease, the liver becomes inflamed and swollen.
- Fibrosis – If inflammation is untreated, healthy liver cells are replaced by scar tissue (fibrosis). Once those cells are gone, the liver can’t regenerate them. If liver disease is detected at this stage, it may be possible to slow down or halt its development. Many people don’t experience symptoms until their liver is seriously damaged.
- Cirrhosis – Cirrhosis is critical, permanent scarring. Years or even decades can pass between the second and third phases of liver disease, presenting a window to get treatment.
- Liver Failure – This is the total malfunctioning of the liver and is the final stage of cirrhosis. The liver can no longer repair itself and can’t be treated. At this stage, a liver transplant is the only course of action.
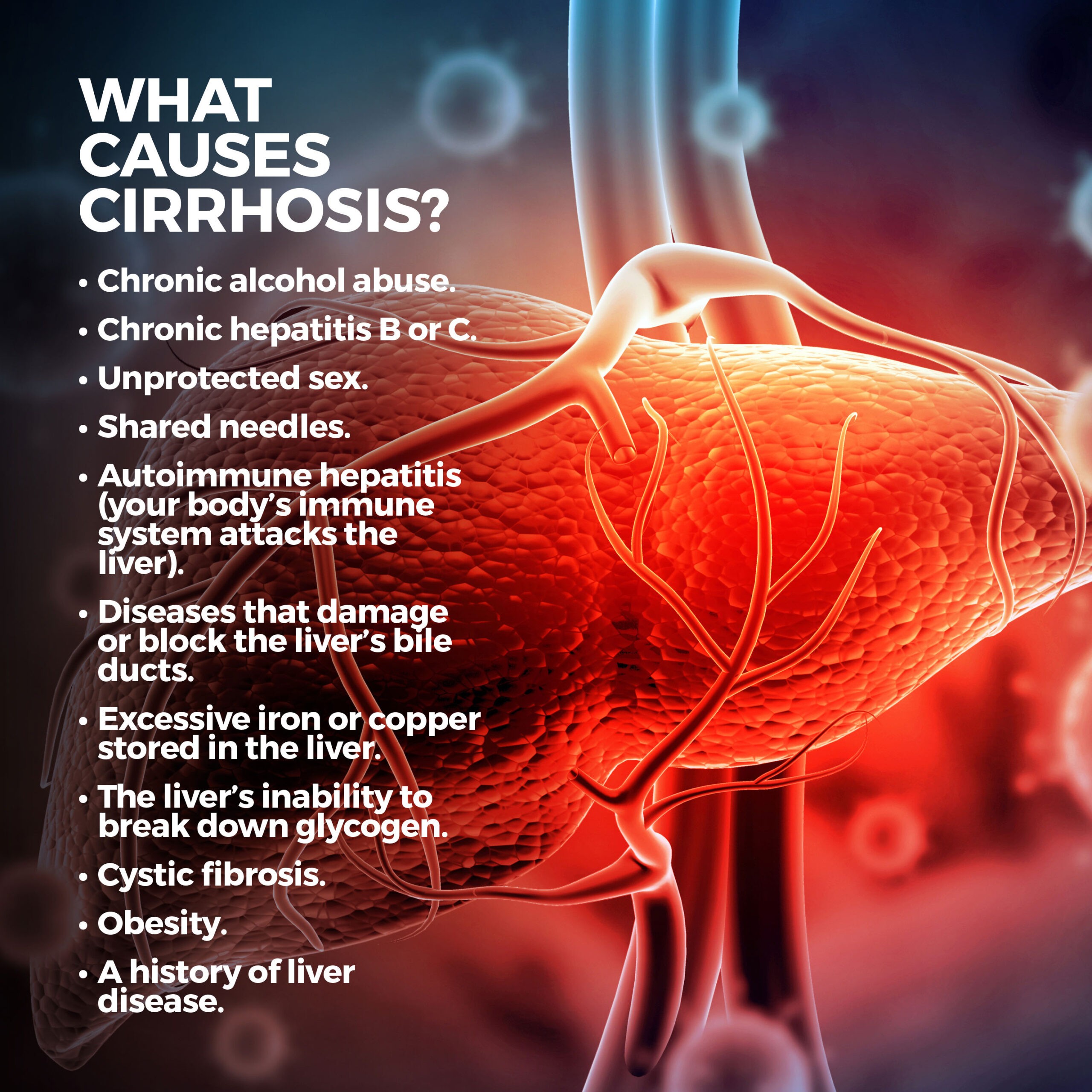
What Causes Cirrhosis?
Many things can lead to cirrhosis. The condition is mainly caused by:
- Chronic alcohol abuse.
- Chronic hepatitis B or C.
Others include:
- Unprotected sex.
- Shared needles.
- Autoimmune hepatitis (your body’s immune system attacks the liver).
- Diseases that damage or block the liver’s bile ducts.
- Excessive iron or copper stored in the liver.
- The liver’s inability to break down glycogen.
- Cystic fibrosis.
- Obesity.
A history of liver disease.
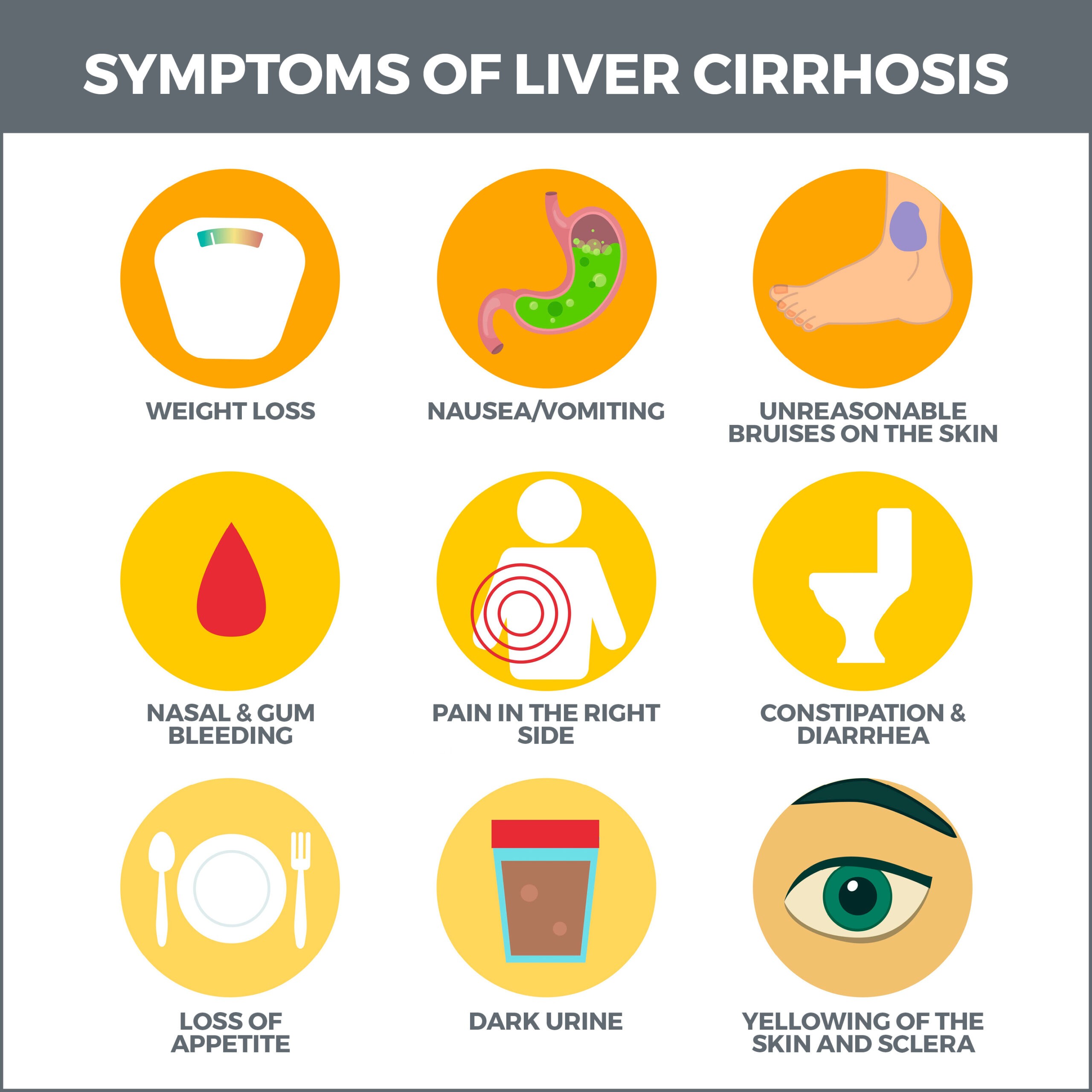
What are the Symptoms of Cirrhosis?
The symptoms of cirrhosis are different for each phase of the condition. In the early stages, they may mimic symptoms of other diseases. These early symptoms include:
- Weakness.
- Fatigue.
- Fever.
- Nausea.
As liver function decreases, other symptoms develop, including:
- Jaundice.
- Itchy skin.
- Swollen legs, feet, and ankles, caused by fluid retention.
- Spider-like blood vessels.
- Red palms.
- Easy bleeding and bruising.
- Fluid buildup in your abdomen.
- Brown or orange urine.
- Pale bowel movements.
- Bloody stools.
- Confusion, slurred speech, drowsiness.
- Unexplained weight loss.
Cirrhosis can also induce liver pain, including a stabbing or throbbing sensation. Pain can also be caused by cirrhosis-induced swelling from fluid retention and spleen enlargement.
How is Cirrhosis Diagnosed?
To diagnose your condition, your doctor will perform a physical exam to look for cirrhosis symptoms. If cirrhosis is suspected, they may order tests.
Blood tests can detect:
- Raised enzyme levels indicating inflammation.
- High iron levels indicating harmful iron buildup.
- Raised liver enzyme levels related to inflammation.
- Low sodium levels.
- Low levels of blood-clotting proteins.
- Autoantibodies.
- High white cell count, indicating an infection.
- Low sodium levels.
- High levels of bilirubin – a fluid that helps digest food. A damaged liver can leak bilirubin into your blood.
- High creatinine levels. Creatinine is a waste substance produced by the breakdown of muscle cells. A healthy liver removes creatinine from the blood.
Imaging tests create detailed pictures of the inside of your body. They can reveal the texture, size, and shape of your liver, as well as the extent of scarring and the amount of fat in the organ. These tests include:
- Magnetic Resonance Imaging (MRI) – This test uses radio waves, large magnets, and a computer to provide images of your liver. MRIs do not use radiation (x-rays).
- Computerized Tomography (CT scan) – Computerized tomography uses x-rays and a series of images to create a three-dimensional view of your liver.
- Abdominal Ultrasound (sonogram) – You may have seen this test used to view the insides of pregnant women. A gel is spread on your abdomen, and a transducer is moved over the area. Sound waves bounce off your liver and produce an image of the organ on a computer screen.
- Endoscopic Retrograde Cholangiopancreatography (ERCP) – This procedure utilizes x-rays and an endoscope (a flexible, lighted tube outfitted with a camera) to detect liver problems. A contrast dye is also added so that the details of the liver become more visible.
A biopsy extracts a liver tissue sample, so it can be examined with a microscope to confirm a diagnosis or identify the severity of damage or enlargement.
When is a Transplant Necessary?
If your liver failure is severe, you may need a transplant. The organ comes from a live or recently deceased donor. After the transplant, the liver can grow to normal size. The liver is the only organ that can regenerate.
Before this procedure, you’ll be assessed by several experts to determine whether you’re eligible for a transplant.
Some of these criteria include:
- All other options have been unsuccessful.
- You and your family, friends, and significant others accept the risks of this procedure.
- These support systems are completely dedicated to and compliant with the care needed after the transplant. This includes adequate funding for the operation, post-transplant medications, and other healthcare expenses.
You’ll be placed on a national waiting list if approved, which doesn’t involve simply taking a number and waiting to be called. Instead, it itemizes potential recipients by their body size, blood type, and disease severity. The most critically ill candidates are prioritized.
Transplant candidates far exceed the number of deceased-donor livers. Opting for a liver from a living person has a shorter waiting period than the wait for a liver from a deceased donor.
When an organ has become available because a donor has died, you’ll need to go to the hospital to prepare for surgery immediately. If a living person is donating their liver, you will be scheduled to have surgery simultaneously. The donor must be healthy and have a blood type that matches yours. They’ll also take a psychological test to ensure they want to donate their liver.
During surgery, up to 60 percent of the donor’s liver is removed and transferred to the body of someone who has cirrhosis. After approximately six weeks, the donor’s and recipient’s livers will grow and function normally.
Instead of one doctor, you will have a team of medical professionals involved in your transplant procedure.
After your operation, you’ll be taught:
- How to check your blood pressure.
- How to take your medications (including anti-rejection medications).
- When you should contact your transplant team.
- The signs of infection and rejection.
As a natural part of its immune response, your body may regard your new liver as a foreign object and attack it. To thwart this reaction, you must take anti-rejection medications for the rest of your life. Because these medications inhibit immune reactions, they also increase the risk of infections. Most of these infections are treatable.
Contact Us
At GastroMD, we offer expert diagnosis, treatment, and aftercare for cirrhosis and other liver diseases. Contact us today. The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority.



