Hepatitis C
Hepatitis C is a viral infection that can seriously damage your liver or lead to death. The hepatitis C virus (HCV) is called “bloodborne” because it only spreads via contaminated blood. It’s primarily transmitted between people who share needles to inject illegal drugs such as heroin, even if they did so only once or many years ago.
Other forms of hepatitis are hepatitis A and hepatitis B, which are transmitted and treated differently than hepatitis C.
There are two types of hepatitis C: acute and chronic. According to the Centers for Disease Control and Prevention (CDC), approximately 2.4 million Americans have HCV. Although hep C is curable, if left untreated, it can become a chronic liver infection (cirrhosis). Over half of those infected with the virus develop a chronic infection.
Acute Hepatitis C
Acute hepatitis C is a short-term infection. It’s the early stage of the disease. Often, you have no symptoms (asymptomatic), and you don’t feel or look sick. It can stay dormant for decades before symptoms arise. If you do experience symptoms, they may only last one or two weeks after exposure to HCV, and the body will clear the virus on its own. This is called spontaneous viral clearance. According to researchers, more women than men clear the virus untreated.
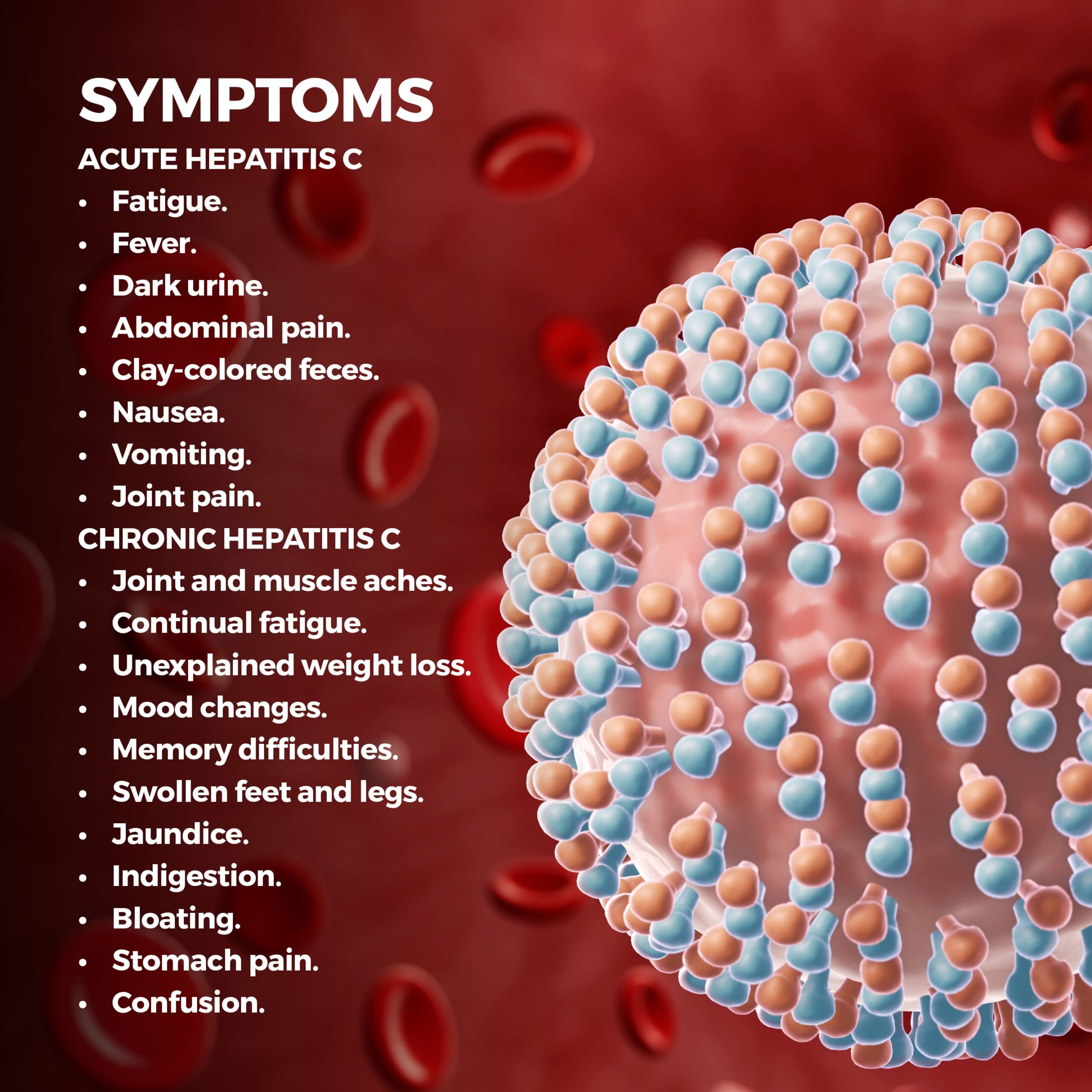
Symptoms of Acute Hepatitis C
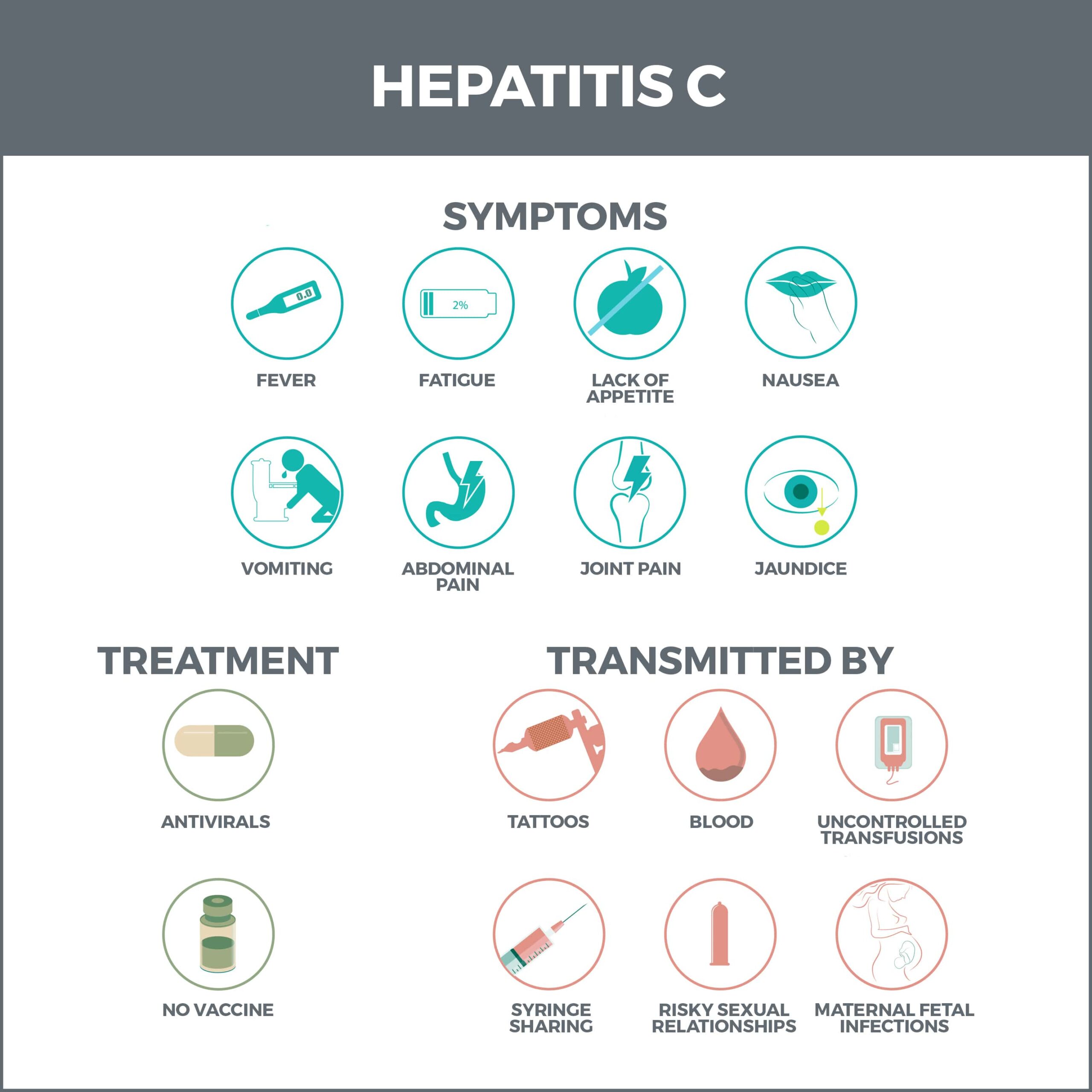
If you have acute hepatitis C, you may not have symptoms or feel sick. When symptoms do occur, they can include:
- Fatigue.
- Fever.
- Dark urine.
- Abdominal pain.
- Clay-colored feces.
- Nausea.
- Vomiting.
- Joint pain.
Chronic Hepatitis C
All chronic hep C infections start as acute. If your body cannot spontaneously clear acute hepatitis C, it will become chronic (long-term) hepatitis C. This happens to 75-85% of infected people. Chronic hepatitis C symptoms can worsen over months or years. Symptoms may be silent (unnoticeable), leaving you unaware of any problem until the virus becomes damaging enough to cause liver disease symptoms. It can take decades for this degree of scarring to occur.
Complications
If hepatitis continues for many years, it can lead to serious complications, including:
- Cirrhosis – Cirrhosis causes scar tissue to replace healthy liver cells. This blocks blood flow, prevents the organ from working properly, and may eventually cause liver failure.
- Liver Failure – Liver failure (end-stage liver disease) happens slowly, for many months or years. A transplant is needed if HCV so severely damages your liver that it stops functioning. But a liver transplant doesn’t cure hepatitis C. Medication is still necessary to manage the infection.
- Liver Cancer – When you have chronic HCV, you risk developing liver cancer. Chronic hepatitis is one of the leading causes of liver cancer.
Symptoms of Chronic Hepatitis C
Chronic hepatitis C symptoms can have long-lasting health effects and may lead to liver cancer and irreversible liver damage. Symptoms include:
- Joint and muscle aches.
- Continual fatigue.
- Unexplained weight loss.
- Mood changes.
- Memory difficulties.
You may also experience symptoms of liver disease and scarring:
- Swollen feet and legs.
- Jaundice.
- Indigestion.
- Bloating.
- Stomach pain.
- Confusion.
How is HCV Spread?
HCV is mainly transmitted through infected blood or bodily fluids containing blood. (Although some individuals get hepatitis C without drug use or blood exposure.) You have a greater risk of contracting HCV if you:
- Share needles for injectable drugs such as heroin. This is the most common way HCV is spread in the US.
- Snort cocaine with shared devices.
- Have had a blood transfusion or organ donation before 1992. This is the year that blood screening was implemented in the United States.
- Were born to an HCV-infected mother.
- Share razors, toothbrushes, nail clippers, or other personal items that can pass blood.
- Have multiple sex partners, engage in unprotected sex, or have a sexually transmitted disease.
- Are a healthcare worker who experienced a needle stick.
- Have had a tattoo or piercing with unsterilized equipment.
- Have HIV/AIDS.
- Have worked or lived in a prison.
- Have hemophilia and were treated with clotting agents before 1987.
- Have been on kidney dialysis.
- Have touched someone’s open sores.
Baby Boomers are particularly vulnerable to hepatitis C because they may have been exposed to the virus before blood screening began in 1992. It’s recommended that anyone born between 1945 and 1965 gets screened for hepatitis C. This group is five times more susceptible to contracting hepatitis C than other age groups.
How Hepatitis C is NOT Spread
There are many misconceptions about how hepatitis C is spread. You cannot transmit or contract it from:
- Kissing, shaking hands, or hugging.
- Breastfeeding.
- Sneezing or coughing.
- Sharing food and drinks.
Hepatitis is only spread through blood-to-blood contact.
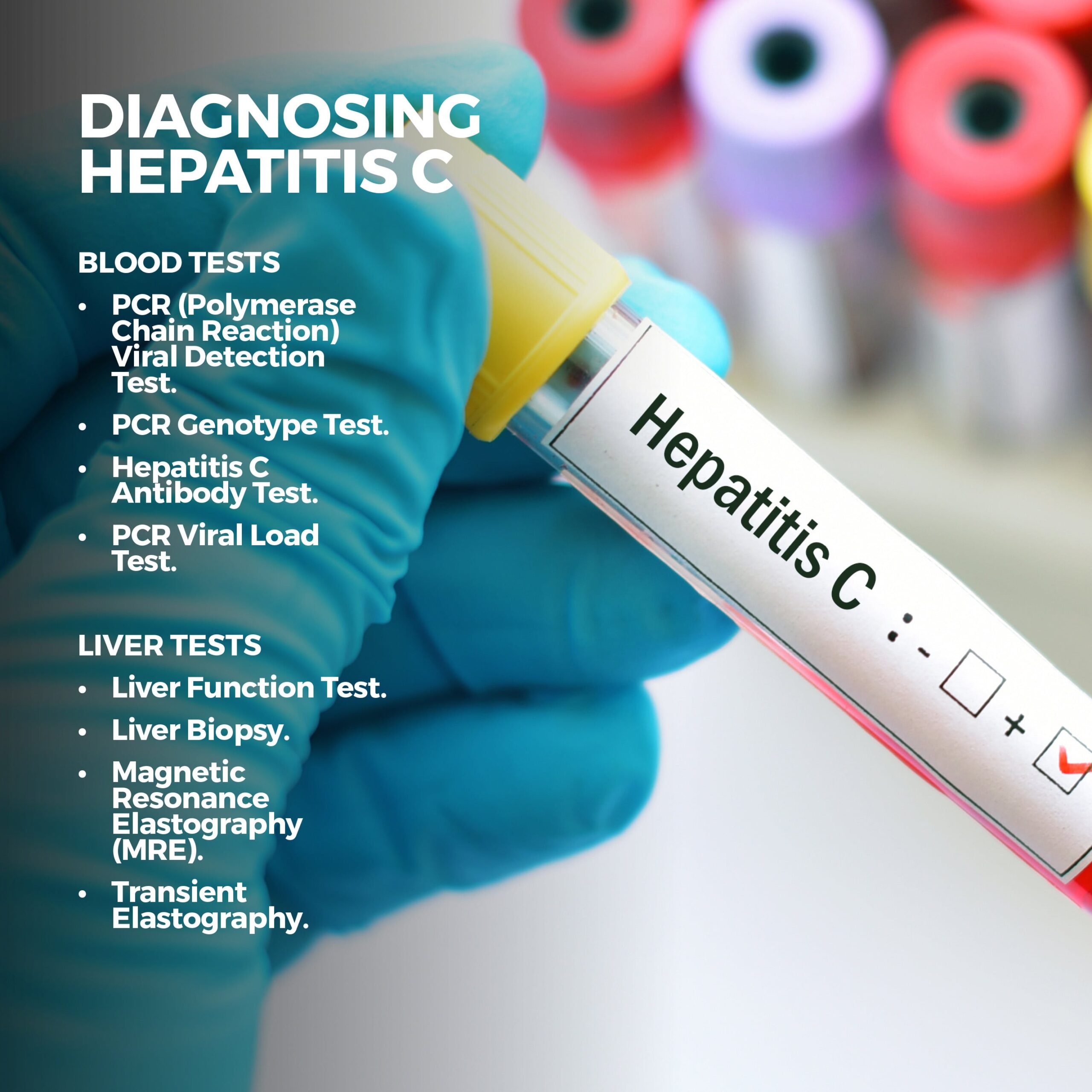
Diagnosis
Multiple blood tests can be done to determine the presence of hep C:
- PCR (Polymerase Chain Reaction) Viral Detection Test – This test can determine whether someone has hepatitis C.
- PCR Genotype Test – A genotype is the strain of virus to which someone was exposed. There are seven hepatitis C genotypes and many subvarieties. Each of these reacts differently to different medications. Genotyping isn’t a remedy but a means of choosing the best treatment options.
- Hepatitis C Antibody Test – Antibodies are manufactured by your immune system to fight foreign substances. Each one fights a specific substance. If you have hepatitis C, your body will make hepatitis C antibodies. A hepatitis C antibody test can determine whether you’re infected by searching for these specific antibodies. This test may take up to three months after exposure to discover these antibodies.
- PCR Viral Load Test – A viral load refers to how much or little hep C virus is in your bloodstream. The test helps doctors gauge whether treatment is lowering virus levels. If a load begins falling, it indicates that treatment is working. Treatment typically lasts 8 to 12 weeks. If a load is completely undetectable at the end of this period, the virus has been cleared, and treatment can be concluded.
Your doctor may also order these liver tests:
- Liver Function Test – If your blood test indicates chronic hepatitis C or possible liver damage, you may be given a liver function test. This test detects elevated liver enzymes.
- Liver Biopsy – A small tissue sample is taken from your liver and tested for cell abnormalities during a liver biopsy.
- Magnetic Resonance Elastography (MRE) – Magnetic resonance elastography is a noninvasive technique that combines magnetic resonance technology with sound waves to determine liver stiffness, indicating liver scarring from chronic HCV.
- Transient Elastography – This noninvasive ultrasound test delivers vibrations to the liver and measures its speed through the organ to determine its stiffness.
Treatment
Although there is no preventative vaccine for hepatitis C, direct-acting antivirals (DAAs) are highly effective in clearing HCV in over 90% of patients. They also have fewer side effects than older options. Even if your treatment is successful, you can still contract another hep C infection, so you must continue avoiding exposure to other people’s blood.
Some types of hepatitis can be treated with a combination of more than one direct-acting antiviral. DAA medications are generally taken twice a day for two to six months and include the following:
- Sofosbuvir.
- A combination of Sofosbuvir and Ledipasvir.
- A combination of Ombitasvir, Paritaprevir, and Ritonavir, taken with or without Dasabuvir.
- A combination of Grazoprevir and Elbasvir.
- A combination of Velpatasvir and Sofosbuvir.
- A combination of Glecaprevir and Pibrentasvir.
If these treatments are ineffective, your doctor may prescribe Riboviria. This medication prevents viruses from multiplying in the body.
Contact Us
It’s important to get hepatitis screening, especially if you’re in a high-risk group. The team of professionals at GastroMD will help diagnose whether you have hepatitis C and create a treatment plan tailored to your needs.
Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in Tampa Bay. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority!



