Diabetes
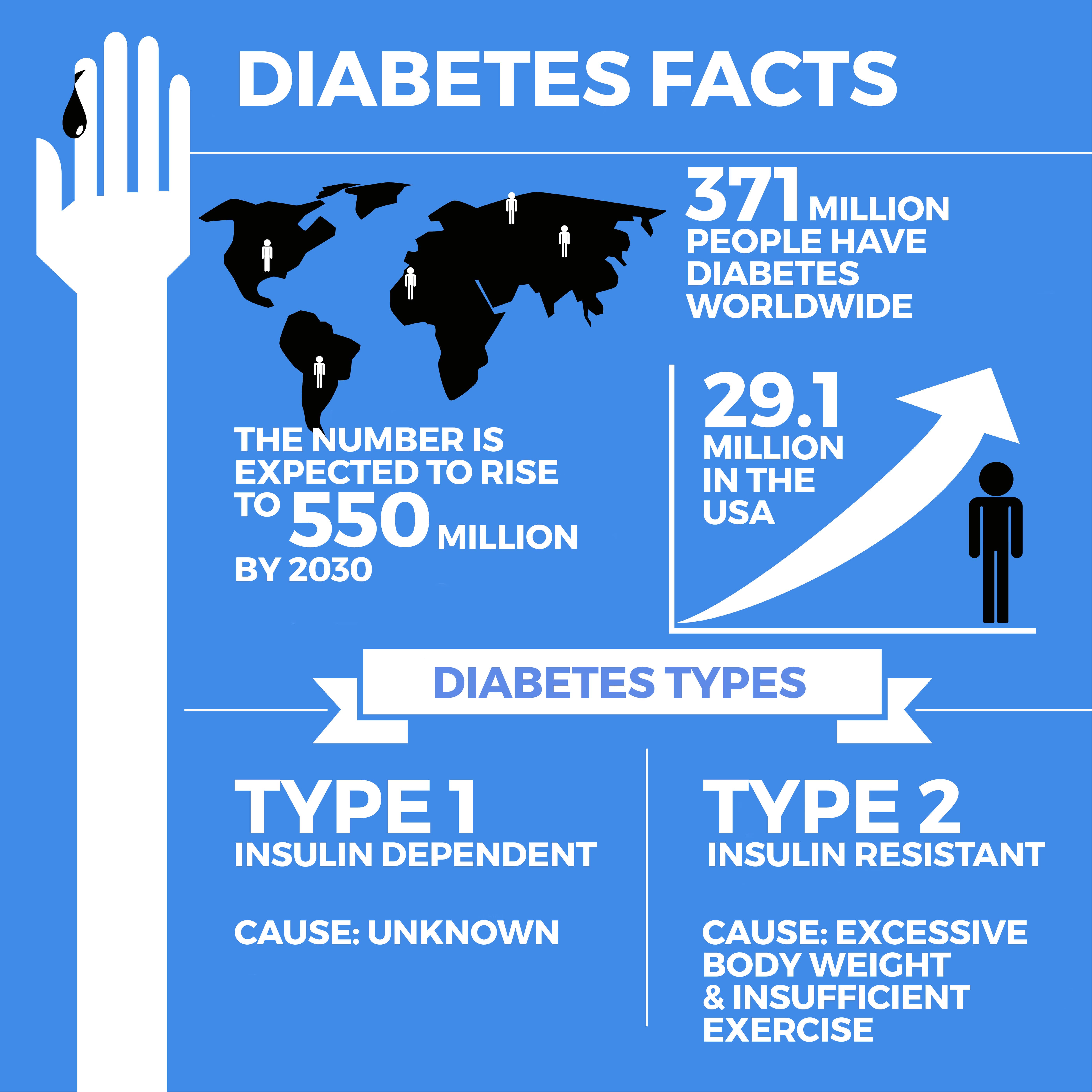
When you have diabetes (diabetes mellitus), your pancreas cannot correctly process or use glucose (sugar) for energy. This causes glucose to build up in your bloodstream, preventing your body from effectively using it. Glucose is a vital energy source for your body’s cells. Diabetes is a serious, chronic (long-lasting) condition, and over time it can lead to kidney failure, heart attacks, blindness, stroke, and lower-limb amputation caused by nerve damage. There is no diabetes cure, but it can be controlled and treated.
What is Diabetes?
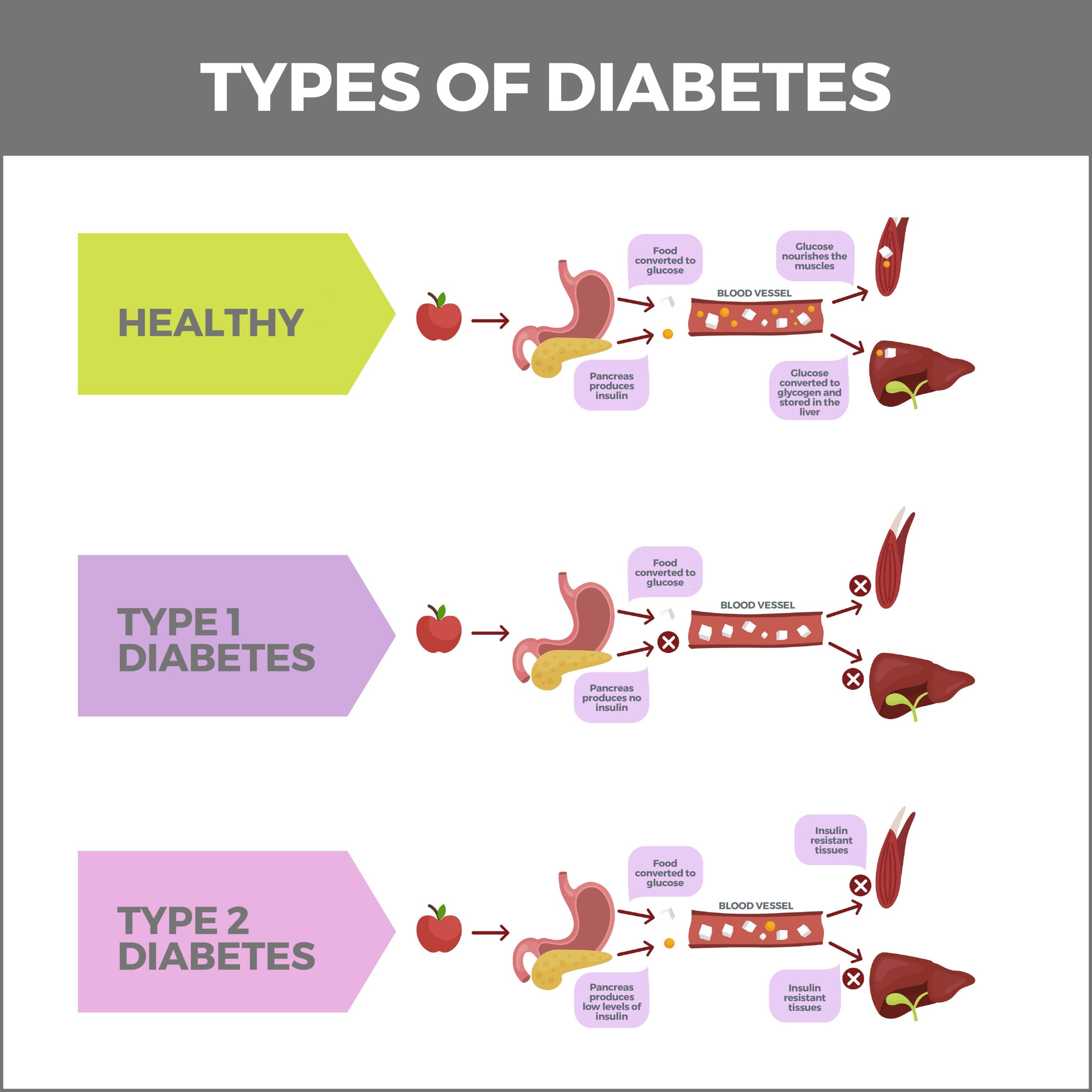
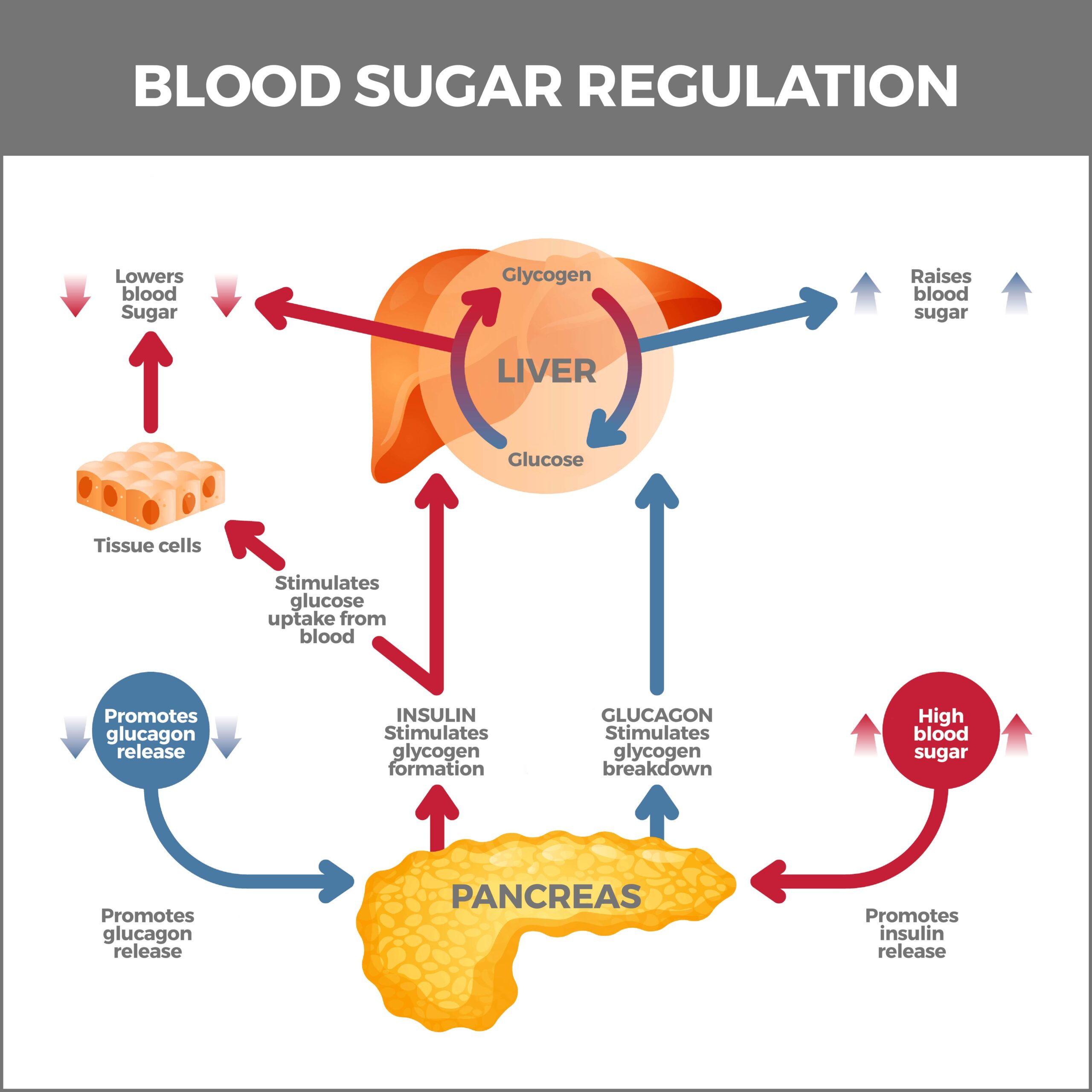
Your body breaks down carbohydrates you eat into sugar and releases the sugar into your bloodstream. As sugar levels rise, your pancreas (an organ located behind your stomach) releases insulin. Insulin is a hormone that lets glucose enter your cells. As cells fill with glucose, sugar levels in your bloodstream become lower. When these levels continue to drop, insulin secretion also decreases.
If you have diabetes, your pancreas doesn’t make enough insulin or any insulin. Diabetes can also occur if your pancreas produces enough insulin, but your body’s cells don’t react to it.
What Are the Types of Diabetes?
There are four types of diabetes.
Type 1 Diabetes
Previously called juvenile, child-onset, or insulin-dependent diabetes, Type 1 diabetes is a chronic autoimmune disease. It’s not caused by diet or lifestyle and can’t be prevented. Although Type 1 diabetes can start at any age, it often affects children or teenagers.
Type 1 diabetes makes your body accidentally attack and destroy your pancreas’ insulin-producing cells (beta cells). Without insulin to help glucose enter your body’s cells, sugar accumulates in your bloodstream. High blood sugar can seriously damage your body. Diabetes Type 1 symptoms happen abruptly, within days or several weeks. Approximately 5-10% of people with diabetes have Type 1 diabetes. People who have Type 1 diabetes must take insulin every day to stay alive. Caucasians in the US are more at-risk for Type 1 diabetes than African Americans, Latinos, or Hispanics.
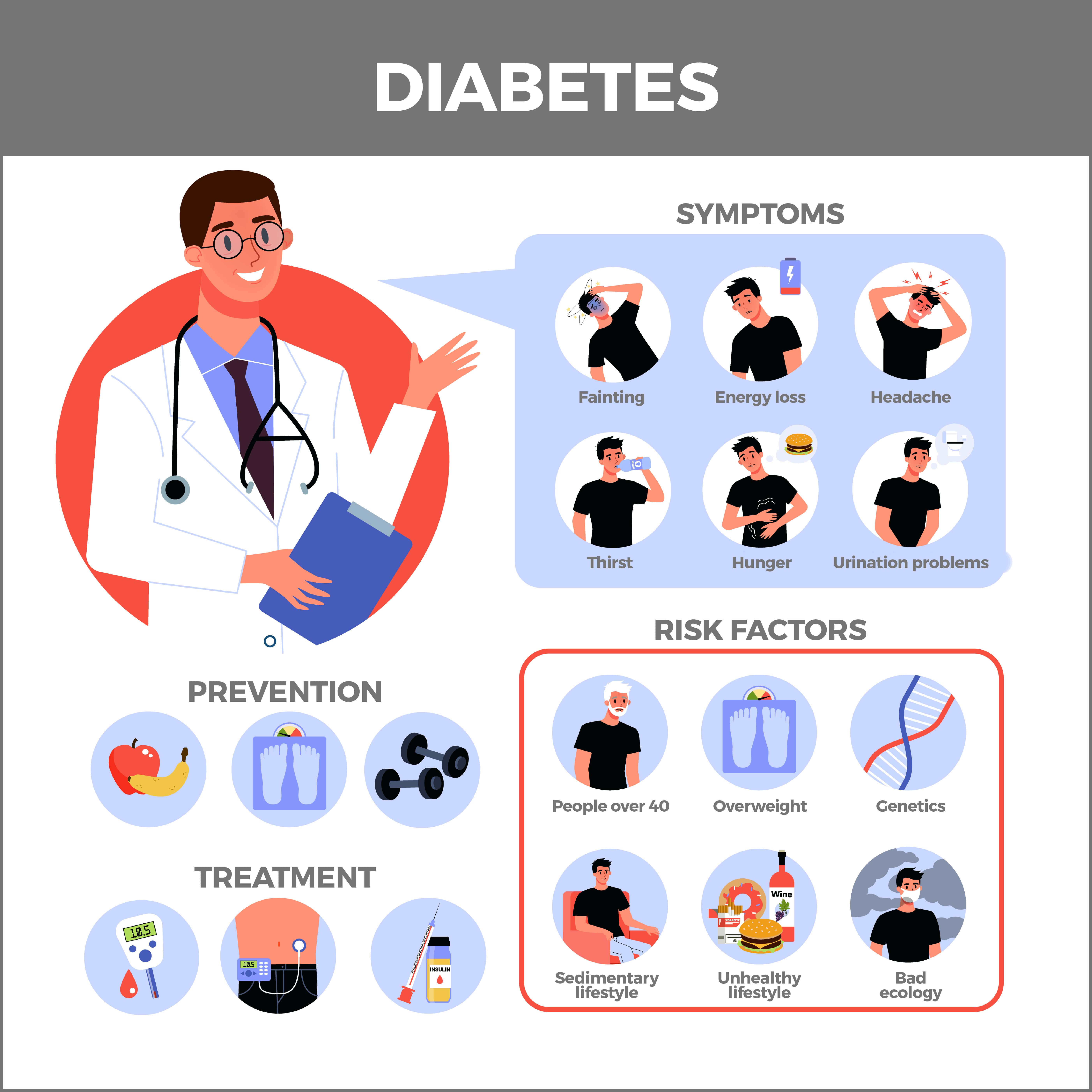
What Are the Symptoms of Type 1 Diabetes?
Type 1 diabetes symptoms are severe and can include:
- Increased hunger.
- Increased thirst and urination.
- Dry mouth and itchy skin.
- Fatigue.
- Blurry vision.
- Unexplained weight loss.
- Slow-healing sores or cuts.
- Numbness or pain in your legs or feet.
- Yeast infections.
One complication of Type 1 diabetes is a dangerous condition called diabetic ketoacidosis (DKA). When your body lacks enough insulin to help blood sugar get into your cells, your liver breaks down fat for energy. This process produces ketone acids. Diabetic ketoacidosis results when ketones inundate your bloodstream and make it too acidic. This buildup can poison your body.
DKA is more likely to occur if you:
- Miss insulin shots.
- Use the wrong dose of insulin.
- Binge drink.
- Have your period.
- Take steroids.
- Use street drugs.
- Have an infection.
Sometimes there isn’t any apparent cause.
What Are the Risk Factors for Type 1 Diabetes?
Type 1 diabetes risk factors include:
- Pancreas injury.
- Family history of the illness.
- Autoantibodies (antibodies that mistakenly attack the body’s tissues).
- Exposure to viral illnesses.
- Bodily stress from surgery or illness.
Although there isn’t a cure for Type 1 diabetes, it can be managed through self-administered insulin injections. The goal of these injections is to keep blood sugar levels close to normal. Before a meal, these blood sugar numbers should be between 80 and 130 mg/dL and less than 180 ml/dL two hours after eating. Mg/dL is a unit of measurement that stands for milligrams per deciliter. It shows the concentration of glucose in a specific amount of blood.
Types of Insulin
To control insulin deficiency, someone with Type 1 diabetes requires daily insulin doses for the rest of their life. There are several types of insulin, including:
- Short-acting insulin – Short-acting insulin begins working about 30 minutes after injection. Peaking at 90 to 120 minutes, it lasts about four to six hours. Short-acting insulin includes Afrezza, Novolin R, and Humulin R.
- Rapid-acting insulin – Rapid-acting insulin starts working within 15 minutes. It hits the peak effect at 60 minutes and lasts about 4 hours. This type of insulin is often taken 15 to 20 minutes before meals. Rapid-acting insulin includes Humalog, Apidra, and Novolog.
- Intermediate-acting insulin – Intermediate-acting insulin starts working in 1 to 3 hours. It peaks at 6 to 8 hours and lasts 12 to 24 hours. Intermediate-acting insulin includes Novolin N and Humulin N.
- Long and ultra-long-acting insulin – These types of insulin may last 14 to 40 hours. They include Lantus, Levemir, and Tresiba.
Injections are administered daily and combine rapid-acting insulin with long-acting insulin.
How is Insulin Taken?
Insulin can’t be taken orally because stomach enzymes would break it down and make it unusable. Instead, it must be taken via:
- Injections – A syringe with a fine needle or an insulin pen can be used to inject insulin. Insulin pens resemble ink pens and are disposable or refillable.
- Insulin pump – An insulin pump is a computerized device that’s the size of a smartphone. It’s worn outside your body and is programmed to deliver insulin through a tube under the skin. If the pump stops working, you’ll always need to keep injectable insulin handy.
Although no form of oral insulin is available, clinical trials are underway.
Type 2 Diabetes
Type 2 diabetes (previously known as adult-onset or non-insulin dependent diabetes) happens when the body can’t effectively use insulin (insulin resistance), and your pancreas doesn’t make enough insulin. It’s the most common type of diabetes. Type 2 diabetes usually results from inactivity or obesity. It can strike at any age but more typically affects people older than 40.
In its early phase, Type 2 diabetes can be controlled with diet and exercise. But if the disease is mismanaged, the body halts insulin production. After this, people who have Type 2 diabetes also must start taking insulin injections.
Symptoms of Type 2 diabetes are much like symptoms of Type 1 diabetes. They may be less noticeable, and the condition may only be diagnosed months or years after the disease develops.
Blood Sugar Testing
If you have diabetes, self-testing your blood sugar levels is crucial to managing your illness. You can use a continuous glucose meter (a device with a glucose sensor inserted under your skin) or a blood sugar meter that analyzes a drop of blood obtained from pricking your finger with a lancet. Your doctor will determine the target blood sugar range for you based on the following:
- Type and seriousness of your diabetes.
- How long you’ve had it.
- Age.
- Whether you’re pregnant.
- Whether you have diabetes complications.
- General health.
- Other medical conditions.
What Are the Risk Factors for Type 2 Diabetes?
You’re at risk for Type 2 diabetes if you:
- Are physically inactive.
- Are obese.
- Have high blood pressure.
- Have low HDL cholesterol (“good cholesterol”).
- Are 45 or older.
- Have polycystic ovary syndrome.
- Are a smoker.
- Have a history of stroke or heart disease.
- Have a family history of Type 2 diabetes or prediabetes.
Prediabetes
If you have prediabetes, your glucose levels are higher than normal but not high enough to be diagnosed as Type 2 diabetes. Yet, it is still a serious health issue. When you have prediabetes, you risk developing Type 2 diabetes, stroke, and heart disease. You can prevent or delay prediabetes from becoming Type 2 diabetes with some lifestyle changes:
- Lose 5-7% of your body weight.
- Regularly do moderate-intensity, 30-minute exercises.
- Stop smoking.
- Eat more vegetables.
- Drink more water.
- Know what type of carbs you’re eating. Some can cause an immediate blood sugar spike.
The risk factors for prediabetes are like those of Type 2 diabetes. If you have prediabetes, your doctor will check your blood sugar every 12 months to make sure you don’t have Type 2 diabetes.
Gestational Diabetes
Some pregnant women develop high blood sugar. This is called gestational diabetes. It usually occurs between 24 and 28 weeks and typically goes away after birth. When you have gestational diabetes, hormones released from the placenta can prevent your body from using or making insulin. Weight and genetics may also be factors. Gestational diabetes puts you at risk for Type 2 diabetes and can also put your baby at risk for:
- Weighing nine pounds or more.
- Having low blood sugar.
- Being born prematurely.
- Developing Type 2 diabetes later in their life.
- Being obese as a child or teenager.
Gestational diabetes usually doesn’t have any symptoms. Your doctor will need to do a blood test to detect it.
After your baby is born, your doctor will also have your blood tested every 6 to 12 weeks and then every one to three years to check your blood sugar levels.
What Are the Risk Factors for Gestational Diabetes?
You’re at risk for gestational diabetes if:
- You’re 25 or older.
- You were overweight before you became pregnant.
- You have a family history of prediabetes or Type 2 diabetes.
- You’re Hispanic, African American, Asian-American, or Native American.
Complications of Diabetes
The longer you have diabetes and the less it’s controlled, the higher the possibility of complications. These include:
- Nerve damage (neuropathy).
- Cardiovascular disease.
- Kidney damage (nephropathy).
- Eye damage (retinopathy).
- Hearing problems.
- Foot damage.
- Depression.
- Alzheimer’s disease.
- Mouth and skin problems.
Contact Us
At GastroMD, we’re committed to partnering with you to find the best possible treatment and management plan for your diabetes. Call us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority!



