
Pancreatitis
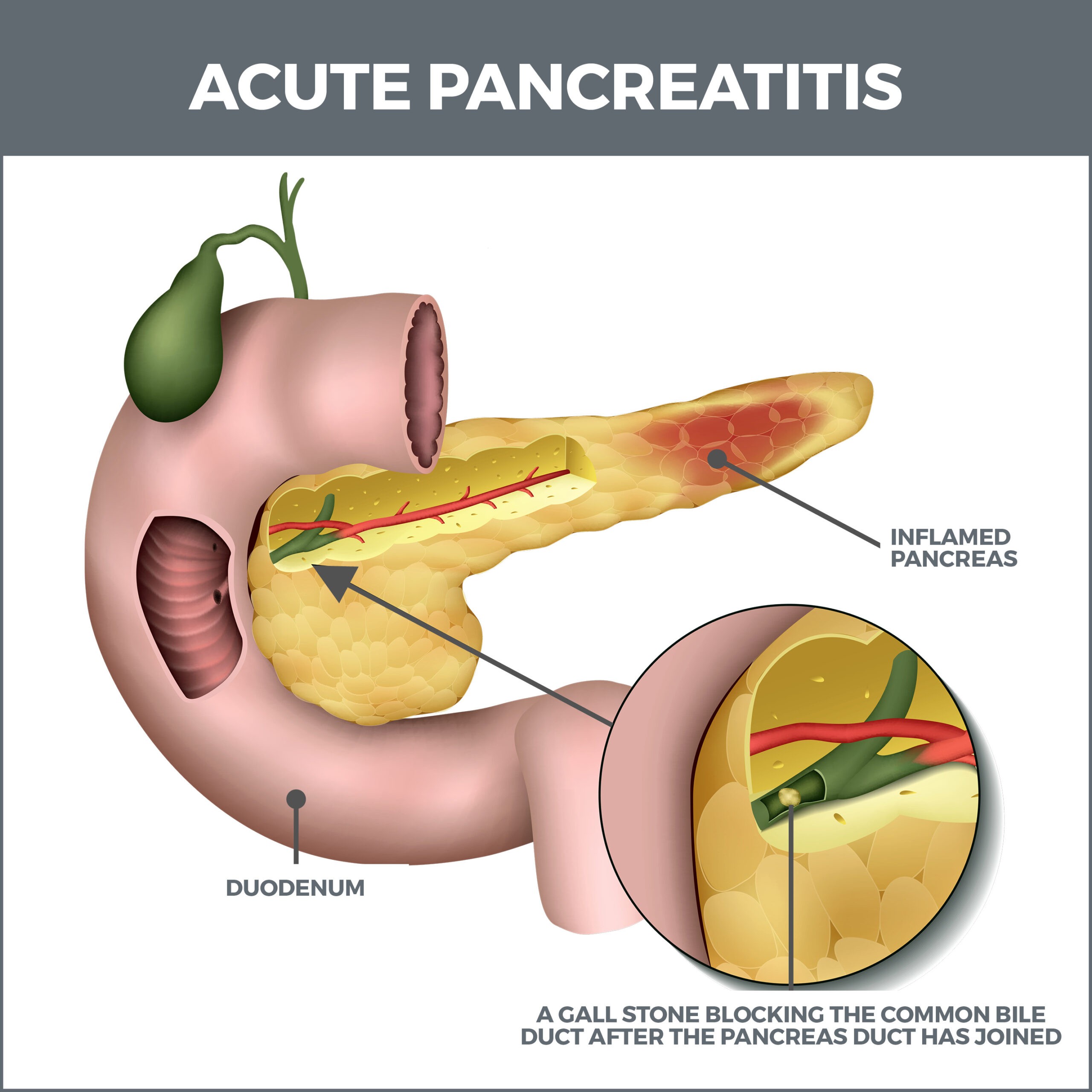
Pancreatitis is an inflammation of the pancreas. It is triggered when the gland’s digestive juices accumulate and start digesting the pancreas itself. The inflammation can be brief and last several days or be drawn out over many years.
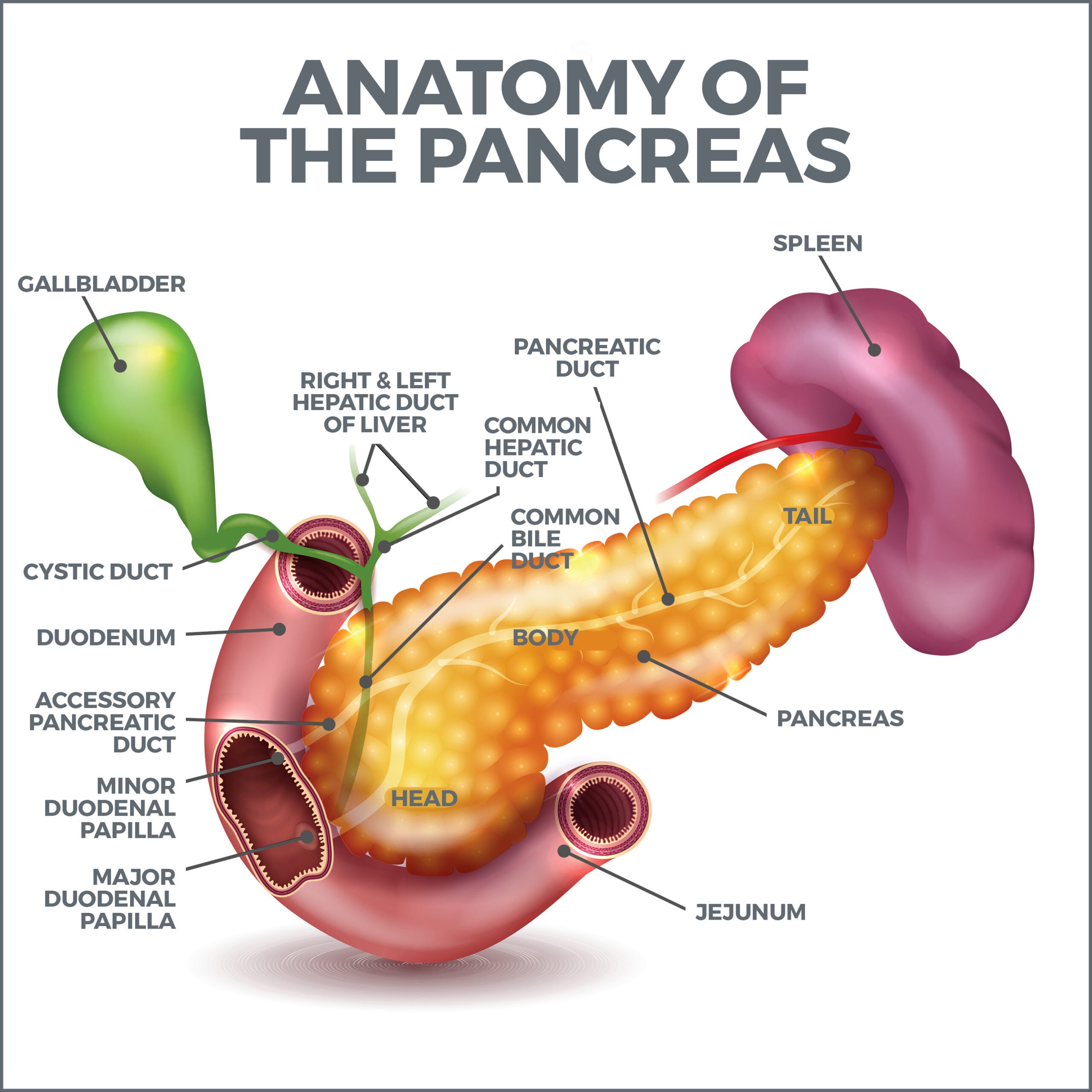
What is the Pancreas?
The pancreas is a long, flat gland located behind your stomach in the upper-left part of your abdomen. It releases juices called enzymes that aid digestion, and it also produces hormones that regulate blood sugar. This gland even produces a natural antacid, sodium bicarbonate. The pancreas releases enzymes and hormones in two ways – through ducts and directly into the bloodstream.
What Types of Pancreatitis Are There?
There are two types of pancreatitis: Acute and Chronic.
- Acute Pancreatitis – Acute pancreatitis is a sudden, brief inflammation. After receiving the proper treatment, most people recover from it within a few days. There are instances in which it can become life-threatening.
- Chronic Pancreatitis – Chronic pancreatitis takes many years to advance and is permanent. It irreversibly damages and scars the gland. Severe pancreatitis can also damage the kidneys, lungs, and heart.
What Causes Pancreatitis?
The same things often cause both acute and chronic pancreatitis:
- Heavy, long-term alcohol abuse. Seventy to 80 percent of pancreatitis sufferers are heavy drinkers.
- Smoking. Smokers are three times more likely to develop the condition than non-smokers. The odds are even worse if you smoke and drink.
- Gallstones.
- Medications including diuretics and estrogen supplements.
- Abdominal surgery.
- Cystic fibrosis.
- Obesity.
- Genetics.
- Infections.
- High blood fat levels.
- Large amounts of calcium in your blood.
- Diabetes.
If doctors are unable to determine the cause of pancreatitis, it is known as idiopathic pancreatitis.
What Are the Symptoms of Pancreatitis?
These are some of the symptoms of acute and chronic pancreatitis. Some of the symptoms for each condition overlap.
Acute:
- Fever.
- Abdominal swelling or tenderness.
- Abdominal pain that intensifies after eating.
- Rapid heartbeat.
- Nausea and vomiting.
Chronic (People with chronic pancreatitis may not experience complications until the condition becomes severe.):
- Abdominal pain that spreads to your back.
- Unexplained weight loss.
- Smelly, greasy bowel movements.
- Diarrhea.
- Nausea.
How is Pancreatitis Diagnosed?
There are several methods for diagnosing pancreatitis. Some are more invasive than others.
- Magnetic Resonance Imaging (MRI) – During an MRI, magnetic waves create highly detailed images of the pancreas for analysis.
- Endoscopic Retrograde Cholangiopancreatography (ERCP) – Using this technique, your doctor can examine the pancreas’ head using a camera mounted on a flexible tube. The tube is guided from your mouth to your small intestine for this procedure.
- Computed Tomography (CT scans) – Computed tomography utilizes computers and X-rays to produce three-dimensional images of your pancreas. A CT procedure shows more detail than a regular X-ray.
- Endoscopic Ultrasound – During this procedure, a special instrument is placed on your abdomen, and sound waves produce images when they’re deflected off your pancreas.
- Biopsy – A biopsy involves the removal of a small tissue sample from your pancreas for examination.
- Blood Test – A blood test can be conducted to determine if you have elevated pancreatic enzymes, amylase, and lipase levels.
Stool Tests:
- Stool Elastase Test: Elastase is an enzyme that is created in a normally functioning pancreas. It helps break down proteins, fats, and carbohydrates. After it does this, it is eliminated in a bowel movement. The stool elastase test measures whether the levels are decreased because of a malfunctioning pancreas. This test is best at detecting severe pancreatic malfunction.
- Stool Lipase Test: This test determines how much fat, or lipase, is in your stool. A damaged pancreas produces excessive lipase.
How is Pancreatitis Treated?
Pancreatitis treatments range from simple dietary changes to hospitalization and surgery.
- Antibiotics – These can be prescribed if your pancreas is inflamed.
- Stents – A stent is a small plastic or metal tube used to keep a duct open. It is used when the pancreas’ ducts are narrowed or blocked.
- Gallbladder Removal – Gallbladder removal is performed when gallstones are responsible for your condition. It is a solution that may be necessary if you’ve had gallstones several times.
- Pancreas Surgery – You may need to have surgery to remove dead or diseased tissue or to drain your pancreas.
- Pancreas Removal – If other treatments fail, you may need to have your entire pancreas removed. This will be followed by islet auto-transplantation. Islets are pancreatic cells responsible for manufacturing hormones. They are transplanted into your liver, where they will resume the process of making and releasing hormones.
- Insulin – If the pancreas is severely damaged, it may stop producing insulin, resulting in Type One diabetes. If this is the case, you will need to take insulin for the rest of your life.
- Fasting and Intravenous Fluids – You will need to stay in the hospital and stop eating for several days to let your pancreas repair itself. You may need intravenous fluids to stay hydrated. If you’re malnourished, you’ll receive nutrition either intravenously or through a tube in your nose. If your condition is severe, you may need to stay in the hospital for three to six weeks and continue receiving these treatments.
- Enzyme Supplements – Your doctor may recommend enzyme supplements to aid digestion. If you suffer from malabsorption, you may also need to take vitamins K, A, E, and D.
What Should I Eat When I’m Recovering From Pancreatitis?
When you’re recovering from pancreatitis, you need to avoid these foods because the gland will struggle to manage them.
- Fried or heavily processed food.
- Red meat.
- Sugary snacks, desserts, and drinks.
- Full-fat dairy, butter, or margarine.
- Caffeine.
- Alcohol.
- Trans-fatty foods.
- Potato chips.
Your doctor may refer you to a dietitian to help you maintain eating habits that will be kind to your pancreas.
Other healthy habits worth adopting include:
- Eat six to eight small meals during the day. This puts less stress on your gastrointestinal tract than consuming three big meals.
- Don’t eat large amounts of fiber at once. This could hamper the digestion of nutrients from the food you eat.
- If you smoke, drink, or do both – stop. If you’re having trouble quitting, join a support group to help you.
Contact Us
Are you experiencing unexplained abdominal pain or other baffling digestive issues? If you are, it’s critical that you turn to a gastroenterologist who can pinpoint what’s causing the problem. The professionals at GastroMD are here to help diagnose the issue and determine a course of action.
Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority.



