Gallbladder Disease
Gallbladder disease encompasses various conditions that affect the gallbladder, including gallstones, cholecystitis, and other diseases that affect its function. Your gallbladder is a small pear-shaped sac located under the liver which plays a crucial role in storing bile produced by the liver and aiding in digestion.
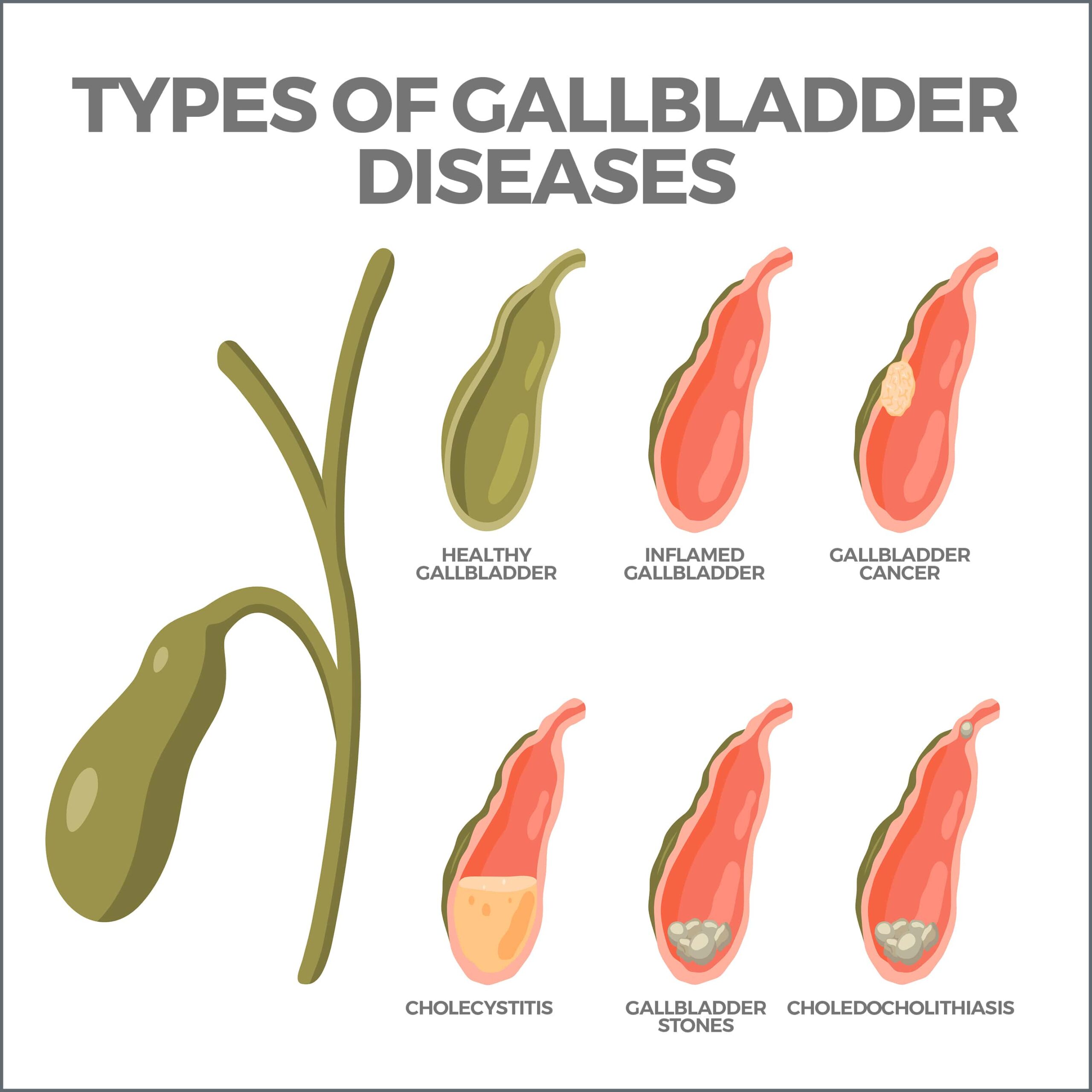
Types of Gallbladder Disease
Gallstones are the most common form of gallbladder disease. They form when cholesterol, bile salts, and calcium solidify and block the passageways to the gallbladder and bile ducts. Gallstones can range from as small as a grain of sand to as large as a golf ball. Other types of gallbladder disease include cholecystitis, choledocholithiasis, acalculous gallbladder disease, and biliary dyskinesia.
Gallstones. Gallstones develop in the gallbladder when substances in the bile, such as cholesterol and calcium, harden. Several factors contribute to the formation of gallstones, including obesity, diabetes, age, hormonal medications, family history, and certain medical conditions like Crohn’s disease. Gallstones can cause various symptoms, including abdominal pain, nausea, vomiting, fever, and jaundice.
Cholecystitis. Cholecystitis refers to the inflammation of the gallbladder and can be either acute (quick and severe) or chronic (continuing over a long time). Acute cholecystitis is typically caused by gallstones blocking the ducts leading to the small intestine. It usually causes severe pain in the upper abdomen, often occurring after meals. Other symptoms can include fever, nausea, vomiting, and jaundice. Chronic cholecystitis occurs when the gallbladder shrinks and loses its ability to store and release bile properly.
Choledocholithiasis. Choledocholithiasis occurs when gallstones become lodged in the neck of the gallbladder or the bile ducts, obstructing bile flow. This condition can cause intense pain in the upper abdomen, fever, chills, nausea, vomiting, jaundice, and pale-colored stools.
Acalculous Gallbladder Disease. Acalculous gallbladder disease is characterized by inflammation of the gallbladder without the presence of gallstones. It is often triggered by severe physical trauma, surgery, burns, autoimmune conditions, infections, or from receiving nutrition intravenously. Symptoms are like those of acute cholecystitis and can include abdominal pain, nausea, vomiting, and fever.
Biliary Dyskinesia. Biliary dyskinesia occurs when the gallbladder fails to function correctly, resulting in lower-than-normal bile storage and release. This condition is often associated with ongoing gallbladder inflammation. Symptoms can include upper abdominal pain after eating, nausea, bloating, and indigestion.
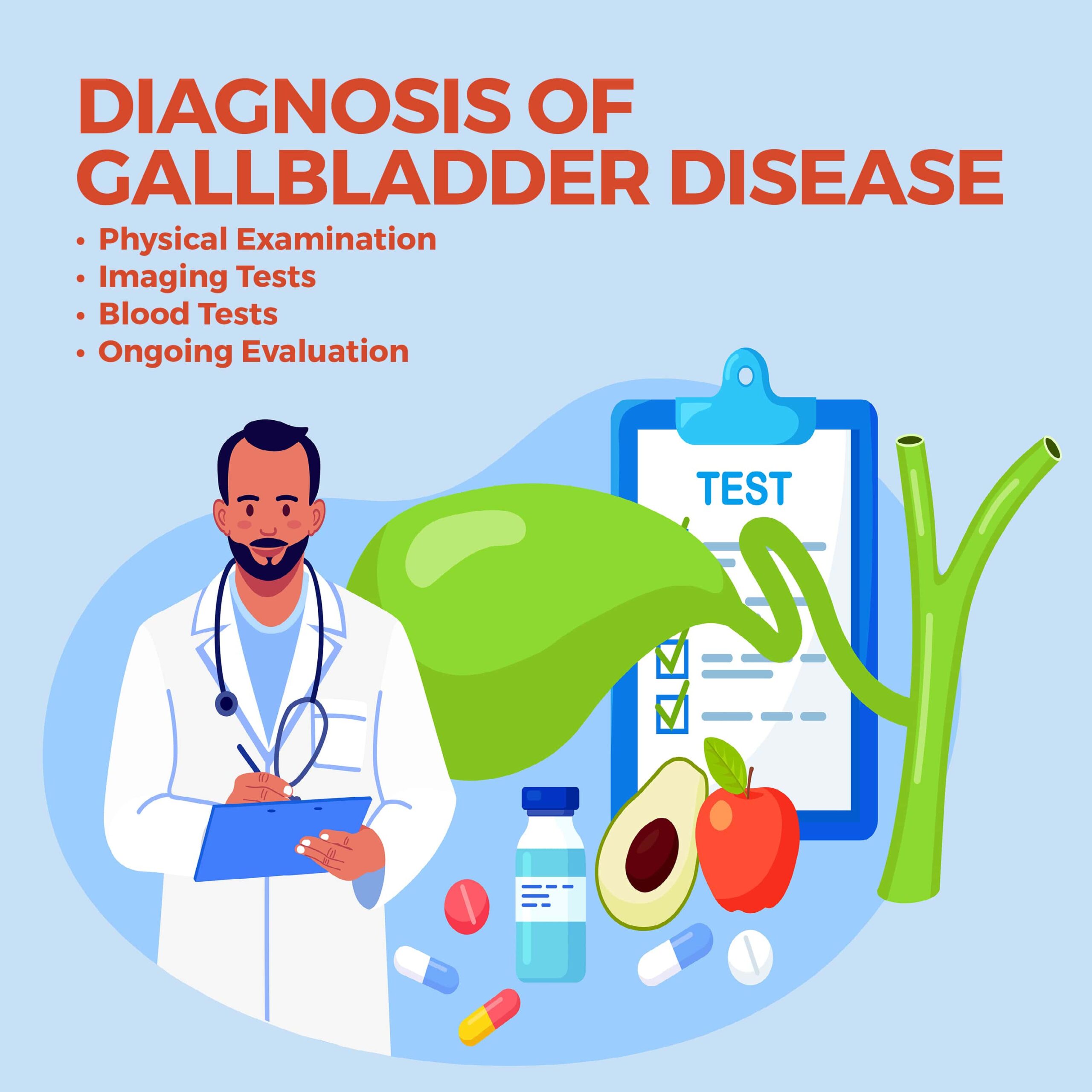
Diagnosis of Gallbladder Disease.
To diagnose gallbladder disease, gastroenterologists typically check a patient’s symptoms, conduct a physical examination, and perform various diagnostic tests. The initial assessment may involve a detailed medical history review to understand the patient’s symptoms and potential risk factors.
- Physical Examination – During the physical examination, your gastroenterologist may use their hands (palpate) on the abdomen to check for tenderness or swelling. They may also check your vital signs, including temperature, heart rate, and blood pressure. These examinations help providers identify any signs of inflammation or infection in the gallbladder.
- Imaging Tests – Imaging tests play a crucial role in diagnosing gallbladder disease. The most common imaging technique is ultrasound, which can detect the presence of gallstones, fluid around the gallbladder, or thickening of the gallbladder walls. If further clarification is needed, your gastroenterologist may recommend additional imaging tests such as CT or MRI scans.
- Blood Tests – Blood tests can provide valuable information about a patient’s overall health and detect abnormalities that may show gallbladder disease. These tests may include a complete blood count (CBC), liver function tests, and tests to measure pancreatic enzymes.
- Ongoing Evaluation – In some cases, if the diagnosis remains uncertain, your gastroenterologist may recommend additional tests such as a hepatobiliary iminodiacetic acid (HIDA) scan or endoscopic retrograde cholangiopancreatography (ERCP). These tests help evaluate the functioning of the gallbladder and bile ducts in more detail.
Treatment Options for Gallbladder Disease
The treatment approach for gallbladder disease depends on the specific condition and its severity. In many cases, surgery is necessary to reduce symptoms and prevent complications. Non-surgical approaches can be effective for certain types of gallbladder disease.
Non-Surgical Treatment
Non-surgical treatments are primarily used for managing symptoms and preventing complications in patients who are unfit for surgery. These treatments may include medications to control pain, antibiotics to treat infections, and lifestyle modifications such as dietary changes to reduce the frequency and severity of symptoms.
Surgical Treatment
Surgery is the most common treatment for gallbladder disease, particularly for gallstones and chronic cholecystitis. The surgical procedure most often performed is laparoscopic cholecystectomy, which is the removal of the gallbladder through small incisions in the abdomen. This minimally invasive approach allows for a faster recovery than traditional open surgery. You can live perfectly normally without a gallbladder, so there aren’t usually any long-term effects from gallbladder removal surgery.
Complications of Gallbladder Disease
Gallbladder disease can lead to complications if left untreated or not managed appropriately. These complications may include gallbladder infections, tissue necrosis, gangrene, bile duct obstruction, and pancreatitis. It is crucial to seek medical attention promptly if symptoms persist or worsen to prevent these complications from occurring.
Prevention of Gallbladder Disease
While some risk factors for gallbladder disease, such as age and family history, cannot be controlled, there are measures you can take to reduce your risk and promote gallbladder health. Many gallbladder problems, especially gallstones, arise from dietary and lifestyle habits. Adopting a proactive approach to your health can support your gallbladder’s optimal function and potentially reduce the risk of diseases.
- Maintain a Healthy Weight – Obesity is a significant risk factor for gallstones and gallbladder disease. By maintaining a healthy weight through regular exercise and a balanced diet, you can reduce their risk of developing gallstones.
- Regular Exercise – Along with helping maintain a healthy weight, regular exercise can aid in proper gallbladder function and reduce the risk of gallstones. Physical activity can help your body metabolize cholesterol, reducing its accumulation in the bile.
- Eat a Balanced Diet – A fiber-rich diet, fruits, vegetables, and whole grains benefits gallbladder health. Rapid weight loss or crash diets can increase the risk of gallstone formation.
- Stay Hydrated – Drinking an adequate amount of water each day helps maintain proper bile flow and prevents the concentration of bile, reducing the risk of gallstone formation.
- Limit Fat Intake – Consuming excessive amounts of fatty foods can increase the workload on the gallbladder and contribute to gallstone formation. Moderation is the key when it comes to fat intake.
- Regular Check-ups – Regular health screenings can catch potential issues early on. If you have a family history of gallbladder disease or other risk factors, regular check-ups can be a proactive measure to ensure your gallbladder remains healthy.
Remember, your gallbladder plays an essential role in digestion. You can support its optimal function by taking proactive steps in your daily life and making informed choices about your diet and overall health. If you experience persistent abdominal pain or other symptoms suggestive of gallbladder disease, seek medical attention promptly. Early diagnosis and treatment can prevent complications and improve outcomes.
Contact Us
Gallbladder disease encompasses various conditions that affect the gallbladder’s function and can cause significant discomfort and complications if left untreated. Understanding the different types of gallbladder disease, recognizing the symptoms, and seeking timely medical attention are crucial for effective management.
Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform many diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority!



