Acute Pancreatitis
Acute pancreatitis is sudden swelling (inflammation) of the pancreas. Some cases are mild and resolve quickly, while others turn into chronic pancreatitis, a dangerous, long-term condition. The pancreas is a small gland located between your stomach and spine. It produces enzymes that flow into the small intestine to help digestion. It also produces hormones that regulate your blood sugar levels. Gallstones and alcohol abuse are the main causes of acute pancreatitis.
What Is the Pancreas?
The pancreas is an organ that is an essential part of digestion. It manufactures hormones, which stimulate stomach acids, tell your stomach when to empty, and control your blood sugar levels and appetite. It also produces juices called enzymes, which break down fats, starches, and sugars.
Each day, your pancreas releases about eight ounces of enzyme-filled digestive juices. Via pancreatic ducts, they empty into the small intestine (duodenum). These enzymes are:
- Amylase – Amylase is an enzyme that breaks down starches into sugar, which gives your body energy. Without amylase, you may get diarrhea from undigested carbohydrates.
- Lipase – This enzyme works with bile – a substance your liver makes for breaking down fat you eat. Without lipase, your body will struggle to absorb fat and crucial fat-soluble vitamins A, D, E, and K. When your body can’t absorb fat, you’ll experience diarrhea and fatty bowel movements.
- Protease – Protease breaks down the proteins you eat. Some people are allergic to undigested proteins.
The pancreas also produces hormones. Unlike enzymes, which are released into your digestive tract, hormones are released into your bloodstream. These hormones are:
- Glucagon – Glucagon is a hormone that’s made in pancreatic cells called alpha cells. Alpha cells make up approximately 20% of your pancreas’ hormone-producing cells. Glucagon regulates your blood sugar levels. Glucagon tells your liver to release stored sugar if your blood sugar drops too low.
- Insulin – Insulin is made in pancreatic cells called beta cells. These cells make up approximately 75% of the pancreas’ hormone cells. Insulin helps your body transform sugar into energy. Your blood sugar levels rise without enough insulin, and you’ll develop diabetes.
- Gastrin and Amylin – Gastrin is mainly produced by the G cells in your stomach, but some gastrin is also made in the pancreas. This hormone stimulates your stomach to produce gastric acid. Amylin, made in beta cells, helps manage stomach emptying and appetite.
What is Acute Pancreatitis?
Acute pancreatitis is a sudden inflammation of the pancreas. It happens when digestive enzymes begin working before your pancreas releases them. This causes the pancreas to digest its own tissue. Most people with acute pancreatitis recover in about a week and have no further issues. In severe or complicated cases, hospitalization may be necessary.
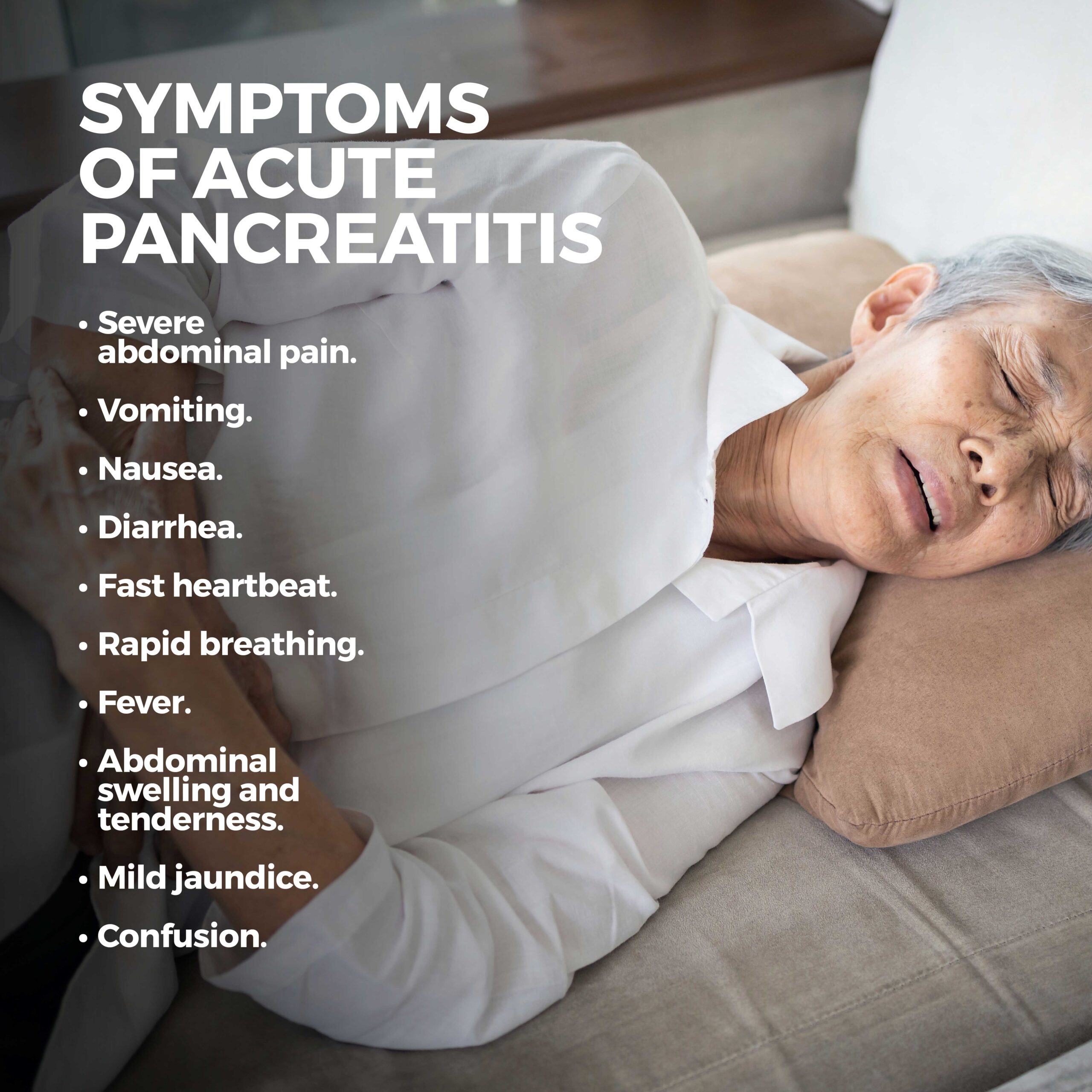
What Are the Symptoms of Acute Pancreatitis?
The main symptom of acute pancreatitis is minor to severe upper abdominal pain. Usually, this pain happens suddenly and may intensify. It can also travel to your back. Although leaning forward, curling into a ball, or sitting upright may make it feel a little better, lying on your back or walking intensify it. If the pain doesn’t stop, see a medical professional.
Other symptoms of acute pancreatitis include:
- Vomiting.
- Nausea.
- Diarrhea.
- Fast heartbeat.
- Rapid breathing.
- Fever.
- Abdominal swelling and tenderness.
- Mild jaundice.
- Confusion.
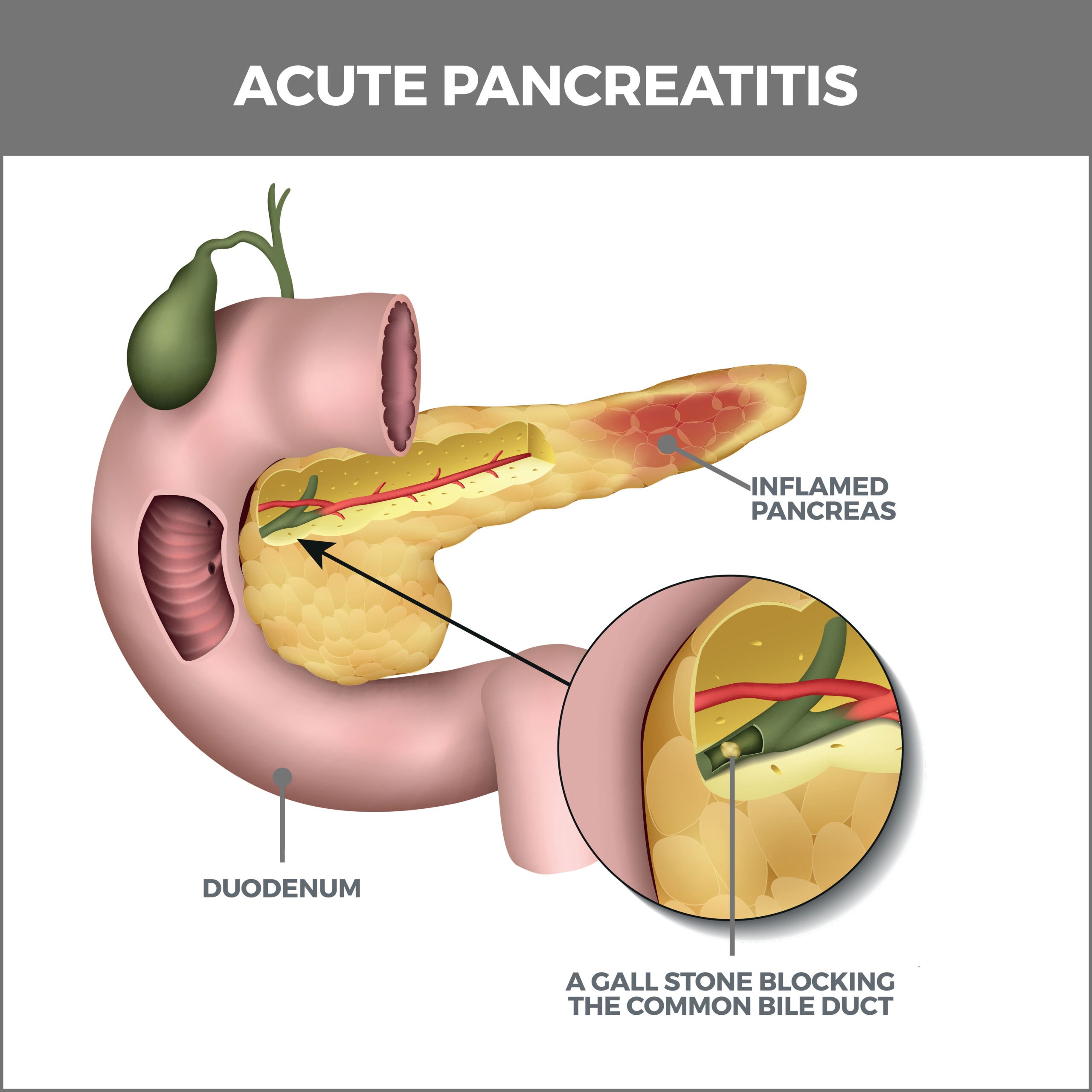
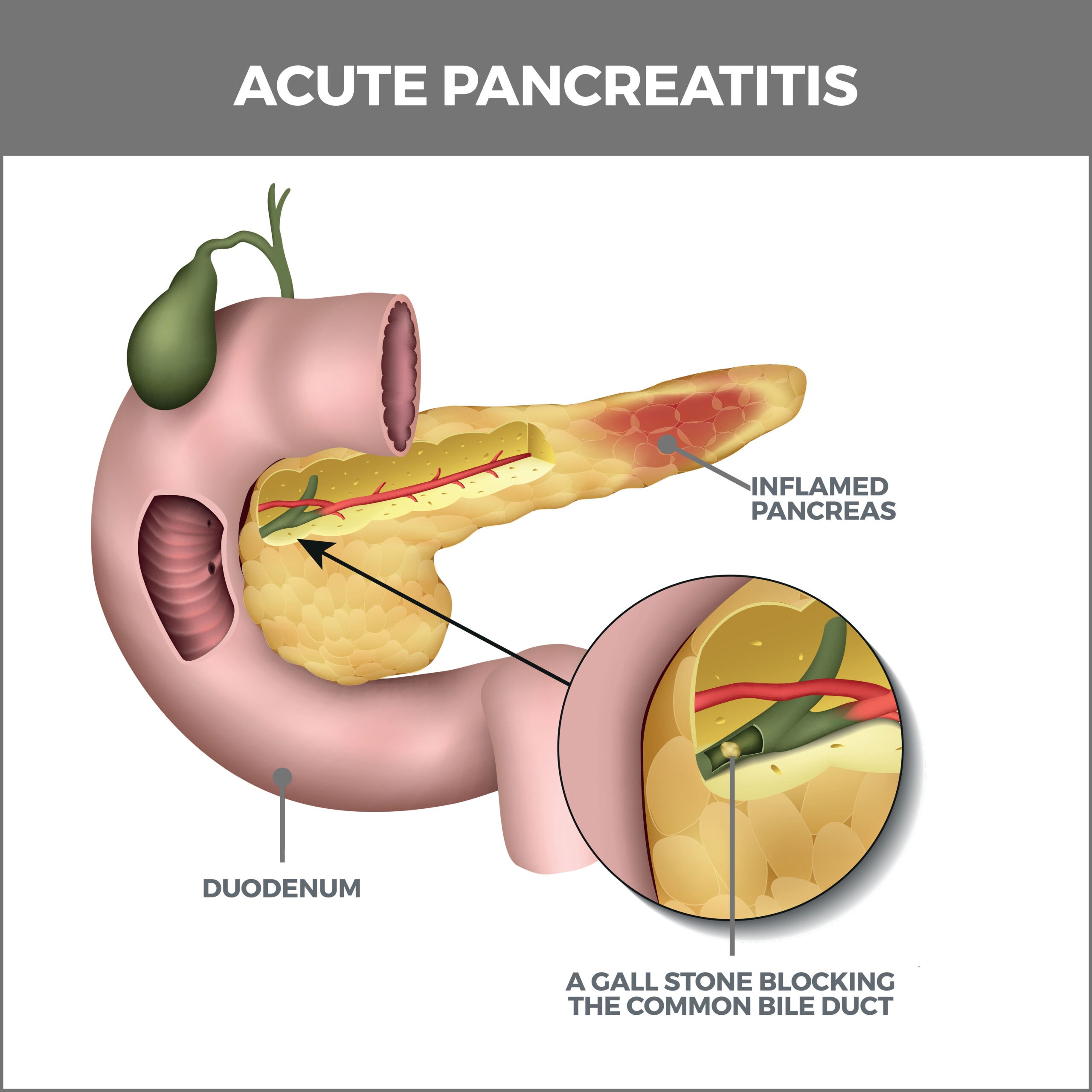
What Causes Acute Pancreatitis?
The two leading causes of pancreatitis are gallstones and alcohol abuse. These conditions account for 60-70% of all acute pancreatitis cases.
- Gallstones – Gallstones are the primary cause of acute pancreatitis. The common bile duct transports bile from your gallbladder into your intestine via the same opening as the pancreatic duct. If a gallstone enters the common bile duct and gets stuck there, it may block the release of pancreatic juice from the pancreatic duct. This traps the enzymes inside your pancreas, causing pressure to build up behind the blockage. Enzymes become activated and start digesting the pancreas’ own tissue.
- Alcohol abuse – Excessive alcohol use is the second leading cause of acute pancreatitis. Although it’s unclear how consuming excessive alcohol causes the pancreas to become inflamed, the two have a definite connection. It’s thought that heavy drinking may cause enzymes to begin digesting the pancreas. Drinking heavily over a short period (binge drinking) may also increase your chances of developing acute pancreatitis.
Less common causes of acute pancreatitis include:
- Trauma or injury to the pancreas.
- Obesity.
- Infections.
- Viruses such as measles or mumps.
- High blood fat levels.
- High triglyceride levels in the blood.
- High calcium levels in the blood.
- Side effects of medication.
- Autoimmune pancreatitis (the immune system attacks the pancreas).
- Genetics – The risk for acute pancreatitis can be passed down from generation to generation due to a mutation in a gene called PRSS1.
- Cystic fibrosis.
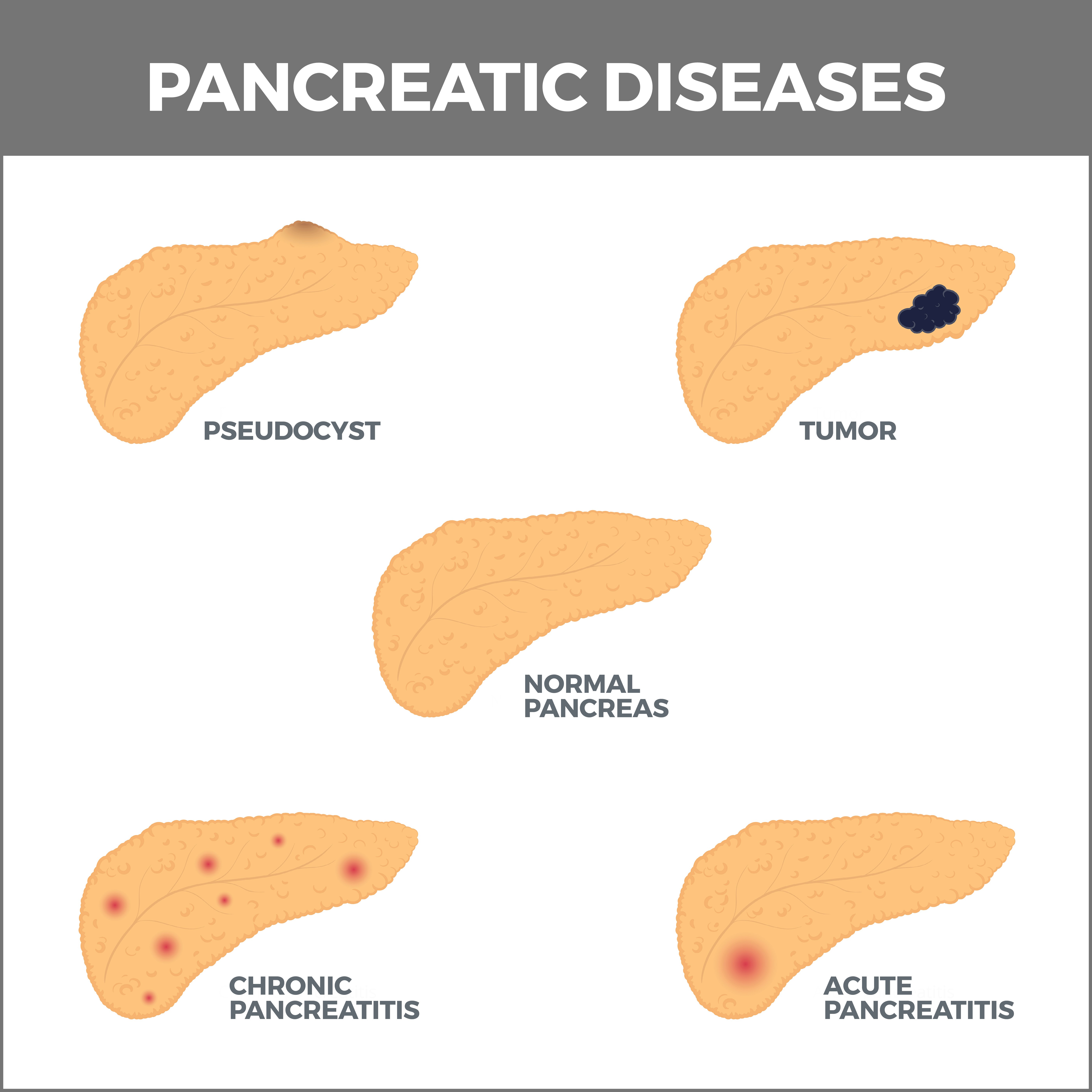
Other Issues Related to the Pancreas Include:
- Pancreatic Cysts – These fluid-filled sacs can grow on the pancreas and are usually not malignant but can be cancerous.
- Exocrine Pancreatic Insufficiency occurs when the pancreas cannot produce enough enzymes.
- Zollinger-Ellison Syndrome – This syndrome causes tumors to develop in the duodenum or pancreas. This causes the stomach to create too much acid.
- Pancreatic Fluid Collections – When the pancreas is inflamed, it can leak digestive enzymes. As the fluid builds up around the pancreas, it can cause symptoms including fever and abdominal pain.
Sometimes, no underlying cause can be determined for acute pancreatitis. This is called idiopathic pancreatitis. Idiopathic pancreatitis happens in about 20% of people with pancreatitis.
How is Acute Pancreatitis Diagnosed?
These tests are used to help diagnose acute pancreatitis:
- Blood Tests – Blood tests look for elevated levels of lipase and amylase, which may be a response to tissue damage.
- Abdominal Ultrasound uses sound waves to produce a picture of your pancreas. It may reveal gallstones in the gallbladder or common bile duct. It may also detect swelling of the pancreas.
- Computed Tomography (CT) – During a CT scan, a series of X-rays are taken to build a detailed picture of your pancreas. This test helps detect pancreas inflammation. During this scan, a patient is injected with a contrast agent, which makes the X-ray images look clearer. This is useful for making an accurate diagnosis and detecting complications.
- Magnetic Resonance Imaging (MRI) – During this procedure, radio waves and strong magnetic fields create detailed images of the inside of your body.
- Magnetic Resonance Cholangiopancreatography (MRCP) – This is a particular magnetic imaging test that can also determine if there are any problems with the bile duct and pancreatic duct.
- Endoscopic Retrograde Cholangiopancreatography (ERCP) – This test helps doctors see the pancreatic and bile ducts and remove gallstones that may be blocking them.
- Sphincter of Oddi Manometry – The sphincter of oddi is a muscle that regulates the flow of pancreatic juices and bile. The procedure lets your doctor see whether it’s opening and closing correctly.
Treatment
If your condition doesn’t clear up on its own, you’ll need to be hospitalized and receive the following:
- IV (intravenous) fluids – Pancreatitis causes dehydration, so it’s very important to have your fluids replaced.
- Painkillers – You’ll either take them orally or receive them through an IV tube.
- Tube feeding – If you can’t tolerate eating food by mouth, you may receive food via a tube passed through your nose or stomach (enteral feeding).
- Parenteral nutrition – You may need to receive food intravenously if your pancreatitis is severe.
- Oxygen – You may be given oxygen via nasal tubes.
- Antibiotics.
- Surgery – If gallstones caused your acute pancreatitis, they will likely return. If you have gallstones in your pancreas, you may need to remove them (cholecystectomy) to prevent this from happening again.
- Pancreas procedures – Your doctor may recommend procedures to drain fluid or remove dead tissues.
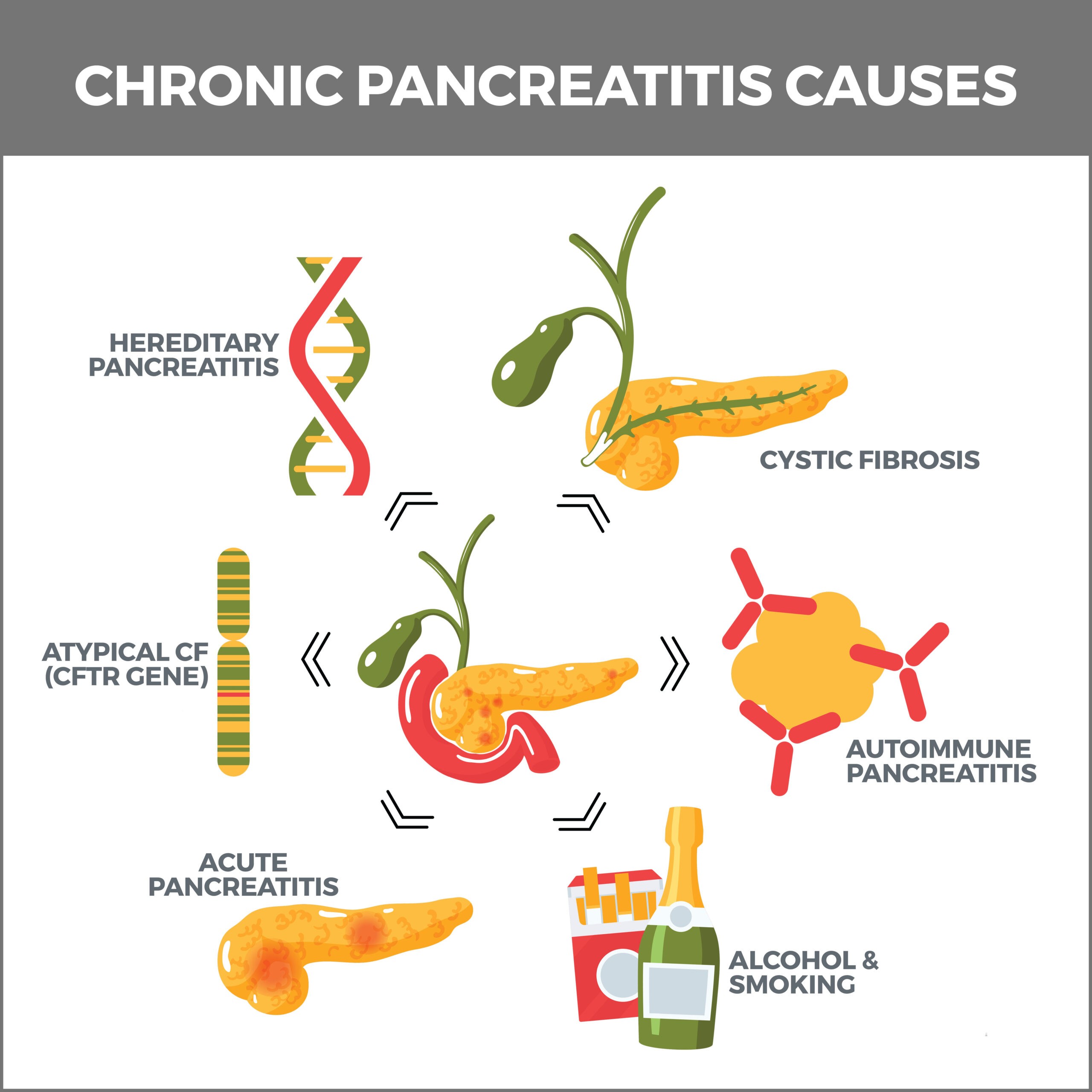
What is Chronic Pancreatitis?
Repeated attacks of acute pancreatitis can lead to chronic pancreatitis. Acute pancreatitis is short-term, but chronic pancreatitis is permanent. When the pancreas is continually inflamed, scar tissue develops over time, hindering the organ’s ability to produce the enzymes needed for proper digestion. This damage is irreversible.
Lifestyle Changes for Acute Pancreatitis
You can aid your recovery from acute pancreatitis by taking steps including:
- Stop drinking alcohol – If you cannot stop drinking on your own, you can get help and support by joining a group such as Alcoholics Anonymous, getting one-on-one talk therapy, or taking a drug called acamprosate that reduces your alcohol cravings.
- Lower your cholesterol – Lowering cholesterol can reduce the risk of gallstones.
- Stop smoking – If you can’t stop smoking on your own, counseling and medications may help.
- Drink more fluids – Since pancreatitis can cause dehydration, be sure to drink fluids throughout the day.
If you have pancreatitis, you should eat the following:
- Less fat.
- Lean protein.
- Fresh vegetables and fruits.
- Whole grains.
- Low-fat or no-fat dairy.
If you have pancreatitis, you shouldn’t eat:
- Red meat.
- Trans fats.
- Cookies, cakes, and pastries.
- Colas and drinks with added sugar.
- Whole milk.
- Fried foods.
- Butter, margarine, and mayonnaise.
Contact Us
Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in Tampa Bay. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority!



