
Gastroparesis
Most foods leave the stomach and empty into the small intestine in about four hours. But if you have a chronic condition called gastroparesis (“stomach paralysis”), food stays in your stomach too long. This can cause interference with normal digestion or a complete blockage between your stomach and your intestine.
To understand this condition, it’s helpful to first understand the stomach’s function.
How Does the Stomach Work?
The stomach is a hollow, muscular organ that rhythmically contracts to grind food into particles easily digested in the small intestine. After the food you eat is pulverized, the vagus nerve cues your stomach muscles to contract and push food into the small intestine.
As the food is gradually propelled into the intestine, it mixes with digestive juices from the liver, pancreas, and small intestine. This process relies on the steady opening and closing of a muscular opening called the pylorus, located between the stomach and the small intestine.
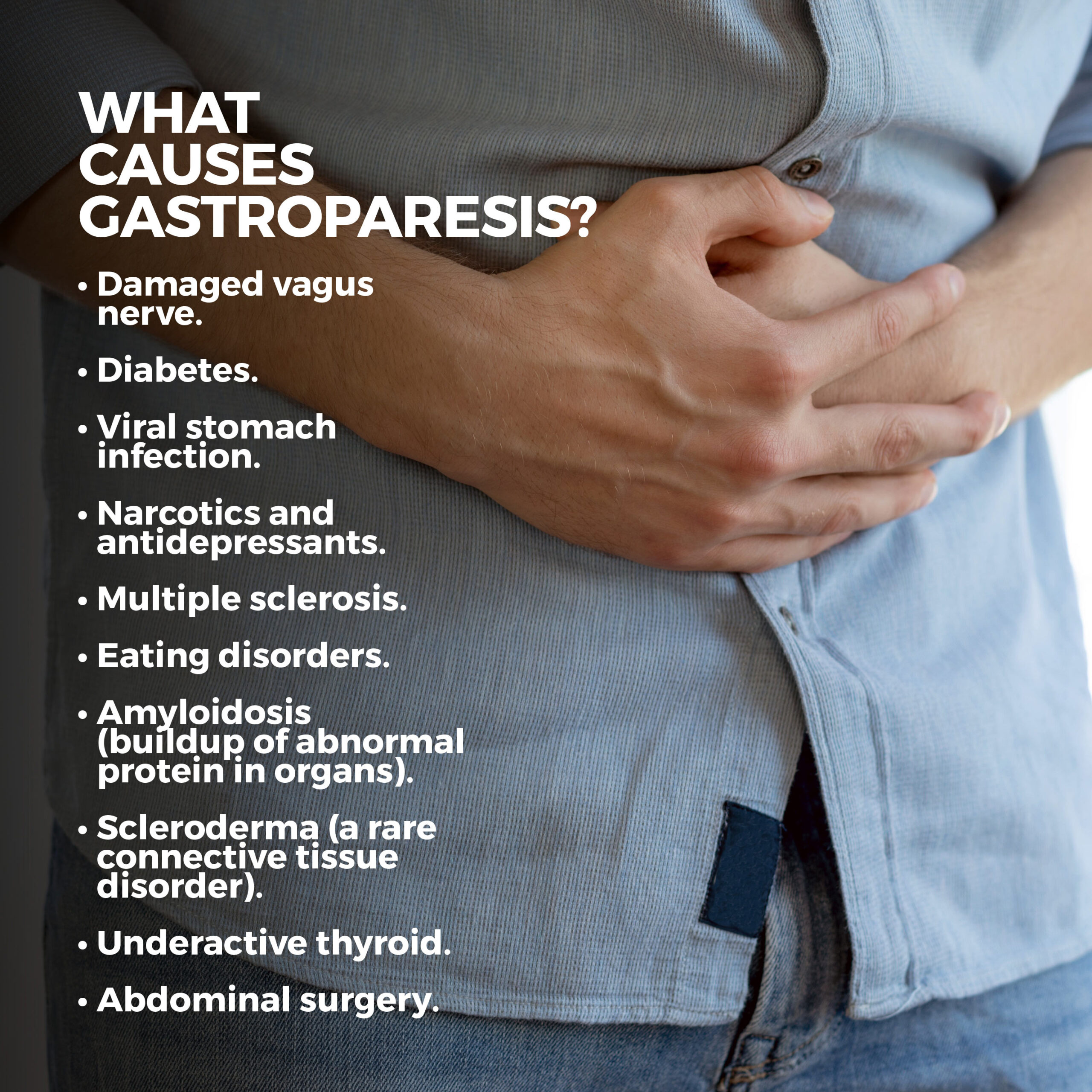
What Causes Gastroparesis?
A damaged vagus nerve triggers gastroparesis. When the nerve is impaired, the stomach muscles and intestinal muscles can’t properly function. This thwarts the normal movement of food from the stomach to the intestines. Gastroparesis typically occurs in diabetics.
Gastroparesis can also be caused by:
- Viral stomach infection.
- Narcotics and antidepressants.
- Multiple sclerosis.
- Eating disorders.
- Amyloidosis (buildup of abnormal protein in organs).
- Scleroderma (a rare connective tissue disorder).
- Underactive thyroid.
- Abdominal surgery.
What Are the Symptoms of Gastroparesis?
The symptoms of gastroparesis range from simple to severe. Although they can happen differently from person to person, they generally include:
- Nausea.
- Vomiting undigested food.
- Feeling full shortly after you start eating.
- Abdominal pain or bloating.
- Heartburn.
- Acid reflux occurring more than two times a week for several weeks.
- Loss of appetite.

What Are the Complications of Gastroparesis?
Gastroparesis is linked to several issues, including:
Malnutrition: Without an appetite, you’ll have a calorie deficit. Additionally, if you’ve been vomiting, your body may be unable to absorb nutrients adequately.
Dehydration: When you can’t keep down liquids, it can lead to dehydration.
- Electrolyte imbalance.
- Weakened immune system.
- Decreased blood pressure.
- Muscle weakness.
- Fermentation.
If food remains in your stomach too long, it may ferment, leading to bacterial growth.
Bezoars: Food that idles in your stomach can solidify into a mass called a bezoar. They can cause vomiting and an upset stomach. Bezoars can be dangerous if they block the entrance to the small intestine.
How Is Gastroparesis Diagnosed?
After reviewing your medical history, your doctor will discuss your symptoms and perform a physical exam. Next, they may order tests such as:
- Blood Tests: Blood tests are the first line of defense in determining a possible case of gastroparesis. These tests can identify infection, malnutrition, diabetes, or dehydration.
- Barium X-ray: You’ll be asked to drink a white, contrast liquid called barium when getting a barium X-ray. Barium coats the stomach and small intestine so that the organs can be seen more clearly on X-rays.
- Gastric Manometry: Gastric manometry examines muscle movement in your stomach and small intestine. Your doctor will guide a slender tube down your esophagus and into your stomach. A wire inside the tube measures your stomach’s electrical and muscular performance while it digests food. This test helps identify lags in digestion.
- Four-Hour Gastric Emptying Test: This test analyzes how long it takes food to travel through your stomach. You will be fed a meal typically consisting of toast with jam, scrambled egg whites, and a glass of water. The eggs will contain a low dosage of radioactive material called a tracer, which helps your doctor see the inside of your stomach. As soon as you’re done eating, a nuclear medicine scanner will take images of your stomach at specific periods for four hours to determine how well food travels through and leaves it.
- Electrogastrography (EEG): An EEG measures the electrical impulses that control your stomach’s contractions. This is done via electrodes placed on the skin of your abdomen. EEG monitors your stomach’s waves and can identify motility issues. The test takes about two hours and is done during fasting, as well as after you’ve eaten.
- Upper Endoscopy: During an upper endoscopy, your doctor will pass a thin, lighted tube outfitted with a tiny camera through your throat and into your stomach. The camera relays images of your stomach’s lining to a monitor for analysis by your doctor. The endoscope can also collect tissue samples, if necessary.
- Wireless Capsule Study: This study involves swallowing a wireless capsule, or SmartPill, that evaluates how quickly your stomach empties and how fast food travels through your small intestine.
- Ultrasound: An ultrasound test uses sound waves to create images of your stomach and intestines. It can also be used to rule out other conditions.
- Carbon Breath Test: During this exam, your carbon dioxide production is tracked through your digestive system. In your doctor’s office, you’ll eat scrambled eggs containing spirulina, a plant-derived protein. Molecules called carbon-13 are placed in the food. This substance can then be measured in samples of your breath as you exhale periodically after eating your meal. These samples can reveal how efficiently your stomach is emptying into your intestine.
How is Gastroparesis Treated?
Gastroparesis can often be managed with simple lifestyle changes, including:
Dietary Changes: A dietician can be extremely helpful for developing a food and nutrition plan that can counteract the symptoms of gastroparesis. They may recommend:
- Reducing carbonated drinks and alcohol.
- Drinking high-calorie liquids.
- Eating low-fat foods.
- Staying well-hydrated.
- Avoiding fiber-dense foods such as spinach, almonds, and popcorn. If you eat vegetables, make sure they’re well-cooked since this breaks down most of their soluble fiber.
- Going to bed no sooner than two hours after eating.
- Eating six small meals instead of three large ones. They may even recommend a few liquid meals.
- Eating smooth-textured food such as applesauce.
Medication: Although medicine can’t cure gastroparesis, it can relieve your symptoms. These medications include:
- Erythromycin: Erythromycin is an antibiotic that makes the stomach contract and moves food along. Its side effects include diarrhea. There’s also a risk of bacterial growth if you take it too long.
- Ondansetron (Zofran): Ondansetron is an antiemetic. An antiemetic is a medication that helps relieve nausea.
- Promethazine (Phenergan): Promethazine is also an antiemetic. It should be used with caution, as it has been associated with neuroleptic malignant syndrome – a potentially fatal condition that may increase your risk for dementia.
- Prochlorperazine (Compro) is used to treat severe nausea and vomiting.
- Metoclopramide (Reglan): Metoclopramide is a medication you take 30 minutes before eating. It stimulates stomach contractions so that food can move along and relieves vomiting and an upset stomach. Reglan’s side effects include diarrhea, anxiety, and drowsiness. A rare side effect is a neurological disorder called tardive dyskinesia.
- Domperidone (Motilium): Domperidone increases the stomach’s contractions. It also eases nausea and vomiting.
If your stomach still isn’t emptying properly, even though you’re medicated, you may need surgery. There are several options available, depending upon the severity of your condition.
- Gastric Electrical Stimulator (GES): A gastric electrical stimulator is a device that is surgically implanted in your stomach. It transmits small shocks to the stomach muscles that prompt contractions.
- Gastric Bypass: During this surgery, a small pouch is formed from the top of the stomach, and the small intestine is divided in half. The intestine’s lower part is connected directly to the pouch. This restricts the amount of food a patient can eat, reducing their gastroparesis symptoms. This option is particularly beneficial for obese diabetics.
- Botulinum Toxin: A botulinum toxin, such as Botox, may be injected into your pylorus, which is the opening between your small intestine and your stomach. This substance relaxes the valve, which keeps it open longer, so your stomach can properly empty.
- Per-Oral Pyloromyotomy (POP): During this procedure, an endoscope is used to cut your pylorus valve so that your stomach can empty more easily.
- Jejunostomy: A jejunostomy is used in severe cases of gastroparesis. A feeding tube is inserted through the skin on your abdomen into your small intestine. Nutrient-dense fluid is delivered into the tube, which will flow directly into your intestine. The nutrients bypass your stomach altogether and enter your bloodstream more quickly.
- Parenteral (Intravenous) Nutrition: If all other methods of treating your gastroparesis have failed, a catheter can be interested into one of your chest veins so that nutrients can go directly through it and straight into your bloodstream. This is generally a short-term solution to quickly control a high-risk case of gastroparesis.
Contact Us
Contact us today. The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority.



