
Eosinophilic Esophagitis
Eosinophilic esophagitis, or EoE, is a chronic immune disease of the esophagus (food pipe). When you have this condition, extra white blood cells called eosinophils (allergy cells) accumulate in your throat and cause inflammation. This damage can produce pain, heartburn, and the development of fibrous tissue and scars that can make swallowing difficult or even cause food to get stuck in your throat.
EoE has no cure, but it is manageable.
What Causes Eosinophilic Esophagitis?
Although the specific cause of EoE is unknown, it is believed to have one or several triggers:
- Airborne contaminants like pollen, pet dander, dust mites, and mold.
- Food allergies associated with wheat, dairy, eggs, soy, peanuts, tree nuts, and seafood.
- Cold or dry climates.
- Asthma, eczema, rhinitis, hay fever, or chronic respiratory disease.
- Gender- Eosinophilic esophagitis affects men three times more than women (ages 20-40).
- Race- EoE is more prominent in Caucasians.
- Genetics- EoE can run in your family.

What Are the Symptoms of Eosinophilic Esophagitis?
EoE can cause a range of symptoms, including:
- Food getting stuck in your throat (impacted).
- Trouble swallowing (dysphagia).
- Nausea and vomiting.
- Malnutrition.
- Weight loss.
- Chest or abdominal pain.
- Food intolerance.
- Poor appetite.
- Feeling full too soon.
- Backflow of food into the esophagus (regurgitation).
- Reflux that is unresponsive to medication.
- Heartburn.
- Bad taste in your mouth.
- Excessive burping.
Esophageal tear, the inflammation caused by EoE, may eventually tear the esophagus’ lining. This is called a perforation.

Eosinophilic Esophagitis in Children
Children and babies are also susceptible to eosinophilic esophagitis. Symptoms for infants and toddlers include:
- Vomiting.
- Inadequate growth.
- Insufficient weight gain.
- Feeding problems and fussiness.
- Reflux that doesn’t respond to medicine.
- Malnutrition.
- Trouble sleeping due to chest or abdominal pain and reflux.
Symptoms for older children include:
- Vomiting.
- Difficulty swallowing.
- Chest or abdominal pain.
- Reflux that doesn’t respond to medicine.
- Food impaction.
- Trouble sleeping due to chest or abdominal pain and reflux.
How is Eosinophilic Esophagitis Diagnosed?
EoE’s high levels of eosinophils in the esophagus can also mimic conditions such as:
- Gastroesophageal reflux disease (GERD).
- Inflammatory bowel disease (IBD).
- Ulcerative colitis.
- Crohn’s disease.
If you have EoE symptoms, it’s important to see a doctor to assess your condition and rule out other conditions accurately.
The following tests are used to diagnose eosinophilic esophagitis.
- Upper Endoscopy – A narrow tube containing a light and camera is passed through your mouth and into your esophagus during this procedure. With this device, your doctor can examine your throat for:
- Swelling.
- Inflammation.
- Vertical furrows (long, narrow channels).
- White spots (plaque).
- Abscesses.
- Strictures (a band of tissue that narrows or blocks your esophagus).
- Sometimes the esophagus can become as narrow as a straw. You may need several endoscopies to determine whether your condition is improving. When performing an upper endoscopy, your doctor may also take several biopsy tissue samples to study under a microscope for signs of inflammation and eosinophils.
- Blood tests – Blood tests can determine total immunoglobulin E levels (an antibody produced when the immune system senses a threat). This antibody usually indicates an allergy or excessive eosinophils.
- Esophageal Sponge – This is a test done in place of an endoscopy. It can determine the seriousness of your esophagus’ inflammation. The test consists of swallowing a capsule attached to a string. When the capsule dissolves, a small sponge emerges. As your doctor slowly pulls the sponge out, it collects esophageal tissue, which can then be analyzed to determine its severity.
How is Eosinophilic Esophagitis Treated?
Although there is no cure for EoE, its symptoms can be managed to minimize the damage to your esophagus. This is done with medication or dietary modifications, including:
- Proton Pump Inhibitors – Proton pump inhibitors are acid-blocking medications that reduce inflammation and minimize reflux symptoms. They are the first line of defense against EoE and can help rule out other conditions that mimic its symptoms. PPIs include Prilosec, Nexium and Prevacid.
- H2 Receptor Blockers (H2 Receptor Antagonists) – H2 receptor blockers are medications that block and reduce acid secreted by your stomach’s lining. This prevents the acid from traveling up the esophagus and causing further damage. Unlike proton pump inhibitors, H2 receptor blockers reduce acid produced at night. These medications include Pepcid, Tagamet, and Axid.
- Corticosteroids – Corticosteroids (fluticasone or budesonide) are liquid medications you can take orally to help control inflammation. Corticosteroids can also be inhaled from an asthma inhaler and swallowed. In some countries, a steroid tablet is available that dissolves on your tongue. It is held in your mouth but not swallowed so that the medicine can gradually travel down your esophagus as it melts.
- Elimination Diet – If you’re on an elimination diet, you stop eating certain foods for several weeks. Then, if you feel better, you reintroduce those foods and drinks one at a time to determine which ones are causing an allergic reaction. There are two types of elimination diets:
- One requires you to have an allergy test and then eliminate the foods and drinks that trigger an allergic reaction.
- The other requires you to eliminate foods that are known to trigger allergies. The most common ones are wheat and dairy. Your doctor will often initially eliminate these foods for about eight weeks. Then, an endoscopy will be performed to determine if the eosinophils have been eliminated.
- Dietary changes can also include eliminating soy, eggs, peanuts, and seafood triggers. While these changes occur, you’ll still eat a healthy diet of fruits, vegetables, and lean meats.
- Elemental Diet – If you’re following an elemental diet, you stop eating all proteins and substitute an amino acid formula. Then you reintroduce foods one at a time to see which ones cause an allergic reaction.
- Dilation – If EoE has severely narrowed your esophagus, it may become challenging to swallow, or food may become stuck. Your doctor may treat this by inserting an inflated balloon or tube to widen it.
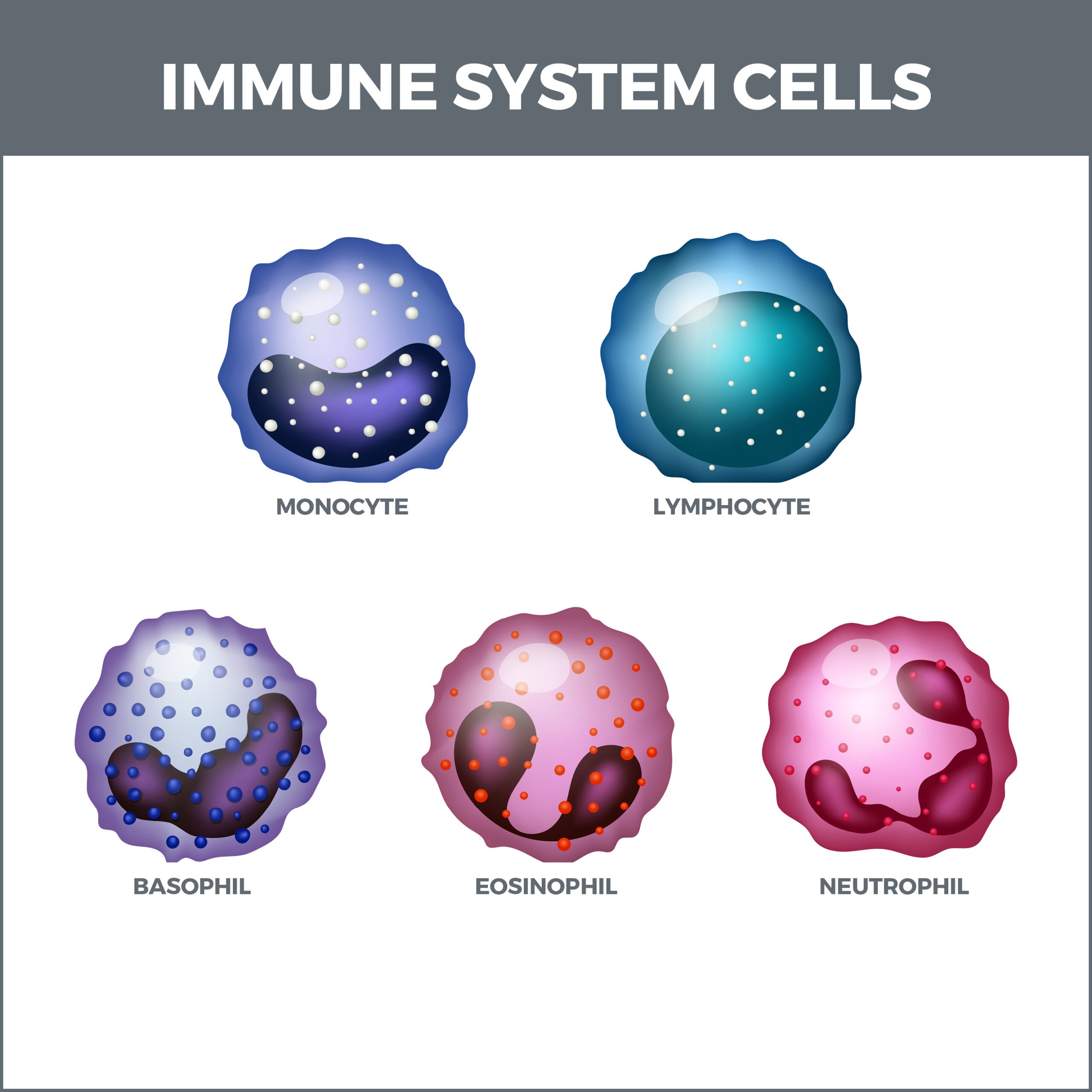
- Differential Eosinophil Count – It may also benefit your doctor to do a differential eosinophil count. This test determines how many white blood cells are present and what kind they are. This includes:
- Eosinophils – Although eosinophils are a destructive part of EoE, they also perform several useful immune system functions (like fending off bacteria and killing parasites).
- Neutrophils – Neutrophils are the most abundant white cells. These cells kill fungi and bacteria.
- Monocytes – Monocytes are one of the largest types of white blood cells. They attack and break down bacteria and germs.
- Basophils – These cells secrete chemicals that bolster your body’s immune response.
- Lymphocytes – Lymphocytes produce antibodies that kill viruses and bacteria.
Should Other Foods be Avoided?
If you have EoE, it’s also good to avoid foods and drinks that provoke heartburn, including:
- Fried foods.
- Fatty foods.
- Spicy foods.
- Alcohol.
- Onions.
- Garlic.
- Chocolate.
- Coffee (caffeinated).
- Tea (caffeinated).
- Soda.
- Tomato sauce.
- Peppermint.
When Should I Call My Gastroenterologist?
Call your doctor if you think you might have EoE and experience:
- Increased trouble swallowing.
- Increased weight loss.
- Stomach pain.
- Increased vomiting.
Support Groups
It may also be helpful to join an EoE support group that you can find via your doctor’s recommendation or an internet search.
Why is Eosinophilic Esophagitis Becoming More Prevalent?
Eosinophilic esophagitis used to be rare. But cases have been rising since the 1990s, with one out of 2,000 people in the United States now affected. This rise in patients may be happening because increased awareness of the condition has produced more diagnoses.
According to Harvard Health, this could also be happening because:
- The Western diet may have adversely altered our microbes.
- Fewer childhood infections may lead to increased allergic conditions.
- Declining amounts of “good” stomach bacteria that protect against allergies.
- Chemical additives, genetically modified crops, pollutants, and food processing.
- Overuse of antacids early in life may increase the chances of developing a food allergy later.
- An uptick in GERD could permit food allergens to affect the immune system.
Contact Us
Although there isn’t a cure for eosinophilic esophagitis, an accurate diagnosis is crucial for treating and managing your condition. GastroMD is one of the leading gastroenterology practices in the Tampa Bay area. We perform several diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere. Patient care is always our top priority!



