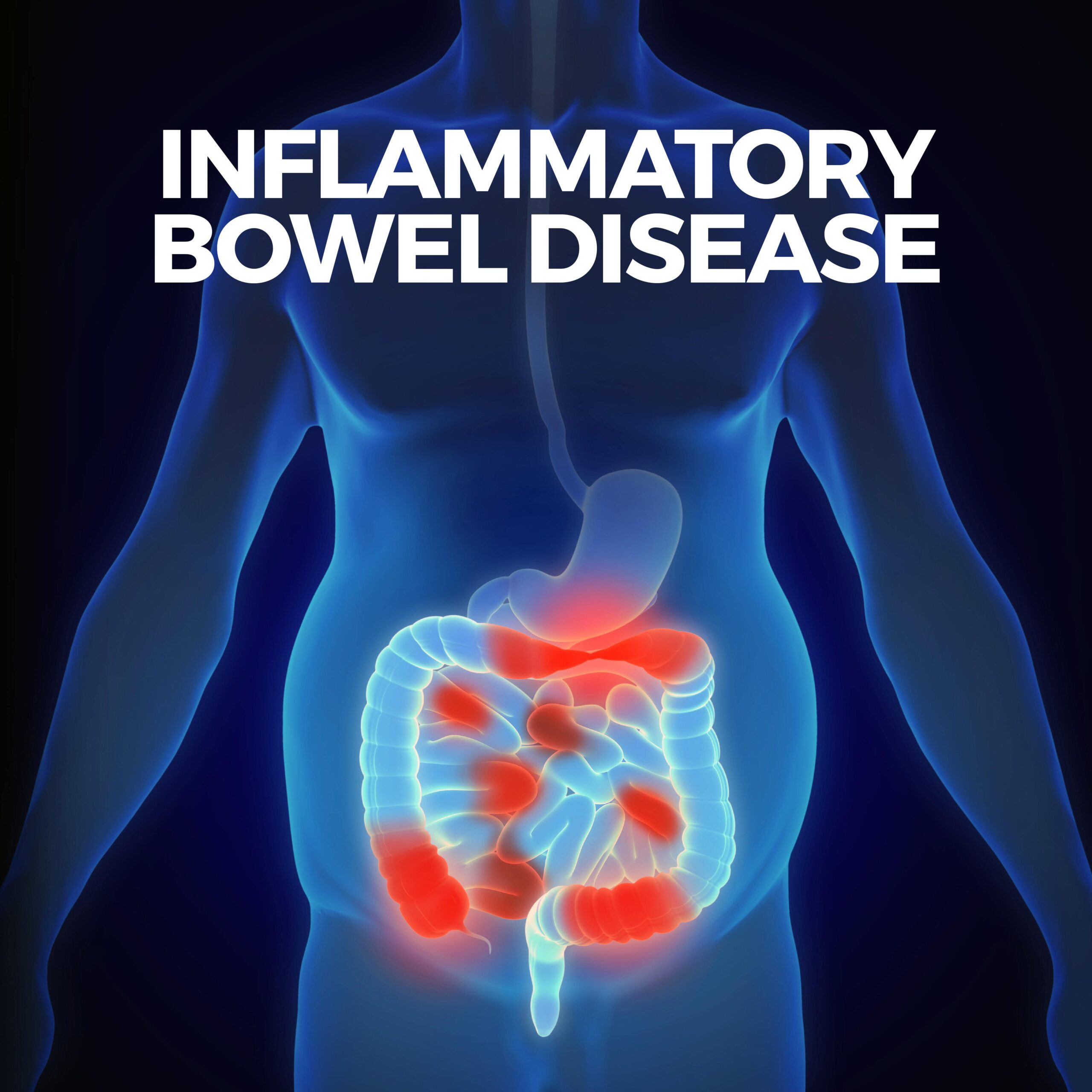
Inflammatory Bowel Disease
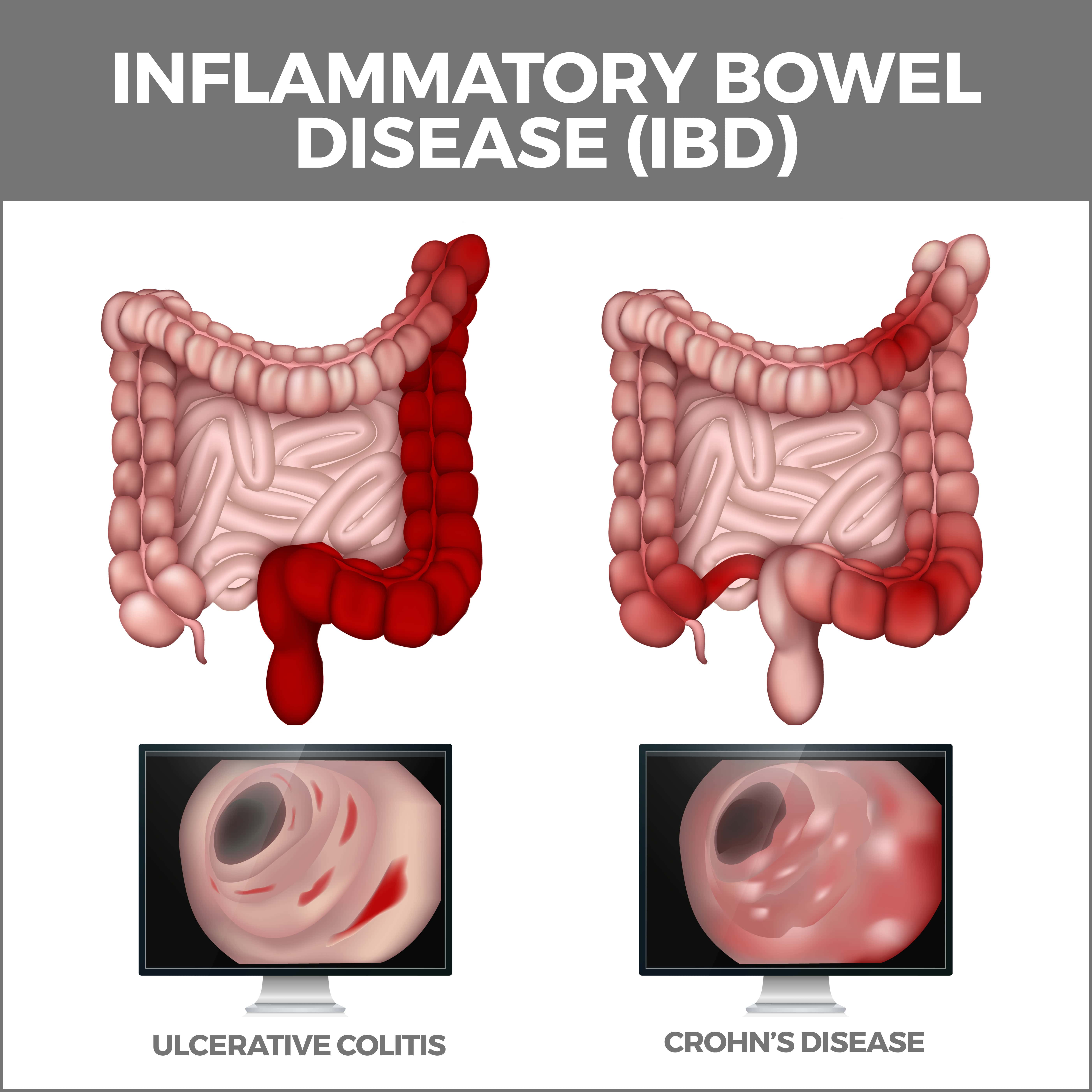
Inflammatory Bowel Disease (IBD) is a chronic and often debilitating condition that affects the gastrointestinal (GI) tract. The two most common forms of IBD are Crohn’s disease and ulcerative colitis. Both conditions cause inflammation in the GI tract, leading to various symptoms and complications. By understanding the aspects of IBD, you’ll be better equipped to manage the condition and get appropriate medical care.
Symptoms of Inflammatory Bowel Disease
The symptoms of IBD vary depending on the severity of the inflammation, the specific form of the disease, and the area of the GI tract affected. Some common symptoms that individuals with IBD may experience include:
- Abdominal pain and cramping: This can range from mild discomfort to severe pain, often accompanied by cramping and bloating.
- Persistent diarrhea: Watery, loose, or bloody stools may occur many times daily, resulting in dehydration and electrolyte imbalances.
- Rectal bleeding: This bleeding occurs because the inflammation and ulceration in the lining of the colon and rectum can cause fragile blood vessels to rupture, leading to the presence of blood in the stool or on toilet paper after wiping. When rectal bleeding is persistent or severe, it can lead to anemia – a condition characterized by a reduced number of red blood cells or low hemoglobin levels.
- Urgent need to have a bowel movement: The sensation of needing to pass stool urgently is a common experience for those with IBD.
- Weight loss and reduced appetite: Inflammation and pain may lead to a decreased appetite and unintentional weight loss.
- Fatigue: Chronic inflammation can cause general feelings of tiredness and fatigue, impacting daily activities and overall quality of life.
- Fever: A low-grade fever may accompany periods of active inflammation.
It’s important to note that symptoms can vary widely from person to person and may change over time. Furthermore, some people with IBD may also experience periods of remission, where symptoms subside temporarily.
Diagnosis
Diagnosing IBD can be challenging, as its symptoms often overlap with other gastrointestinal disorders. To make an accurate diagnosis, your gastroenterologist will likely perform a combination of tests, including:
- Medical history and physical examination: Your gastroenterologist will ask about your symptoms, personal and family medical history, and perform a physical exam to check for signs of inflammation or tenderness in the abdomen.
- Blood tests: Blood tests can help identify anemia, infection, or inflammation markers that may suggest IBD. These tests can also help rule out other conditions with similar symptoms.
- Stool tests: Analyzing a stool sample can help identify the presence of blood, inflammation, or infection. This information can aid in diagnosing IBD and differentiating it from other conditions, such as irritable bowel syndrome (IBS).
- Imaging studies: X-rays, CT (Computerized Tomography) scans, or MRI (Magnetic Resonance Imaging) scans can provide detailed images of the gastrointestinal tract, revealing signs of inflammation or complications associated with IBD. Barium enemas or small bowel follow-through studies may also be performed to visualize the intestines more clearly.
- Endoscopic procedures: Colonoscopy or sigmoidoscopy allows the doctor to examine the interior of your colon and get tissue samples (biopsies) for further analysis. Upper or capsule endoscopy may be used to visualize the upper GI tract in suspected Crohn’s disease cases.
Treatment of Inflammatory Bowel Disease
While there is no cure for IBD, various treatment options can help manage symptoms, reduce inflammation, and prevent complications. Your gastroenterologist will develop a personalized treatment plan based on the severity of your condition and specific needs. Some standard treatment options include:
- Medications: Anti-inflammatory drugs, immune system suppressors, and biologic therapies are commonly prescribed to reduce inflammation and decrease symptoms. Antibiotics may also be prescribed to address infections or complications related to IBD.
- Nutrition therapy: A balanced diet, sometimes including dietary supplements or enteral nutrition, can help provide essential nutrients and reduce symptoms. Sometimes, a temporary liquid diet may be recommended to allow the bowel to heal. Your gastroenterologist may also suggest specific dietary changes to help manage your symptoms, such as a low-residue or lactose-free diet.
- Lifestyle modifications: Managing stress, exercising regularly, and avoiding known triggers can help improve the overall quality of life for individuals with IBD. Quitting smoking, staying hydrated, and getting enough sleep can also improve symptom management.
- Surgery: In severe cases, surgery may be necessary to remove damaged portions of the gastrointestinal tract or address complications such as strictures, fistulas, or abscesses. In some severe cases of ulcerative colitis, a colectomy (colon removal) may be required. A resection of the affected area may be performed in cases of Crohn’s disease.
Living with IBD can be challenging, but you can actively manage your condition by understanding the symptoms, diagnosis, and treatment options available.
Prevention of Inflammatory Bowel Disease
Inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, is a complex and chronic condition with no known cure. Some lifestyle changes and strategies may help manage symptoms, reduce the risk of flare-ups, and promote overall gut health. Here are some prevention tips for IBD:
- Eat a balanced diet: Focus on consuming a well-rounded diet rich in fruits, vegetables, lean proteins, and whole grains. While there is no specific diet for IBD, a balanced diet can help maintain overall health and support gut function. Keep a food diary to help identify foods that may worsen your IBD symptoms. Common trigger foods include high-fat or fried foods, spicy foods, dairy products, and high-fiber foods. Once identified, limit or avoid these foods to reduce the risk of flare-ups.
- Eat smaller, more frequent meals: Consuming smaller, more frequent meals throughout the day, rather than two or three large meals, may help reduce stress on the digestive system and decrease symptoms.
- Stay hydrated: Drink plenty of water throughout the day to stay hydrated, particularly during flare-ups, when diarrhea can lead to dehydration.
- Manage stress: Stress can exacerbate IBD symptoms. Incorporate stress-reduction techniques into your daily routine, such as deep breathing, meditation, yoga, or mindfulness practices.
- Exercise regularly: Engage in regular physical activity to help maintain a healthy weight, reduce stress, and support overall well-being. Consult your doctor to develop an exercise plan tailored to your needs and limitations.
- Quit smoking: Smoking has been linked to an increased risk of Crohn’s disease and can worsen symptoms. Quitting smoking is an essential step in managing IBD and promoting overall health.
- Limit alcohol and caffeine intake: Alcohol and caffeine can exacerbate IBD symptoms in some individuals. Watch your consumption and limit intake if you notice a connection between these substances and your symptoms.
- Stay up-to-date with vaccinations: People with IBD may be at a higher risk for infections. Talk to your doctor about recommended vaccinations and ensure you stay up-to-date with your immunizations.
While these prevention tips can help manage IBD symptoms and reduce the risk of flare-ups, it is important to maintain regular communication with your gastroenterologist to address any concerns and track your condition closely. IBD management often requires a personalized approach based on your specific needs and symptoms.
Contact Us
Gastro MD is committed to providing comprehensive and compassionate care for individuals with gastrointestinal disorders, including IBD. Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area.



