GI Hemorrhages
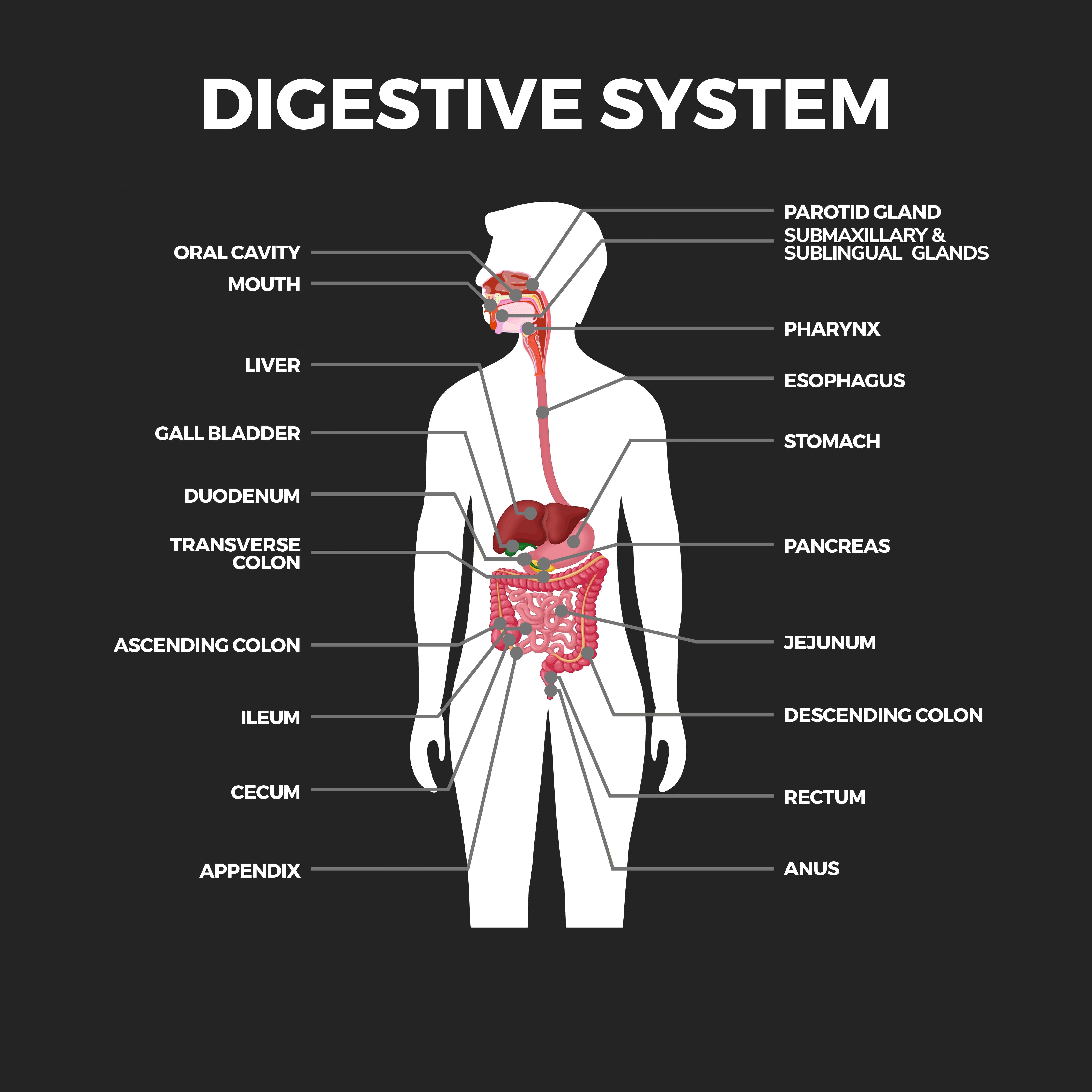
A gastrointestinal hemorrhage, or bleeding, is a condition that occurs anywhere along your digestive tract. This includes the esophagus (food pipe), stomach, small intestine, large intestine, rectum, and anus.
There are two categories of gastrointestinal bleeding: upper and lower. Upper gastrointestinal hemorrhage is bleeding in the esophagus, stomach, and first part of the small intestine. Lower gastrointestinal hemorrhage is bleeding in the lower small intestine, large intestine, rectum, and anus. GI hemorrhage isn’t a disease but a symptom of one or more underlying conditions. A bleeding digestive tract can be minor or life-threatening. Your doctor will help locate the source of the bleeding so that it can be effectively treated.
Types of Gastrointestinal Tract Bleeds
There are five types of gastrointestinal tract bleeds:
- Obscure – A gastrointestinal tract bleed is obscure when a standard endoscopy doesn’t reveal the bleeding’s source.
- Occult – Occult (hidden) bleeding can’t be seen with the naked eye and is discovered through lab tests.
- Acute – Acute hemorrhages are severe and sudden. They need immediate medical attention.
- Chronic – Chronic bleeding is bleeding that comes and goes.
- Overt – With overt bleeding, blood is visible. You may vomit blood that looks red or blood that resembles coffee grounds, have black, tarry stools, or experience rectal bleeding.
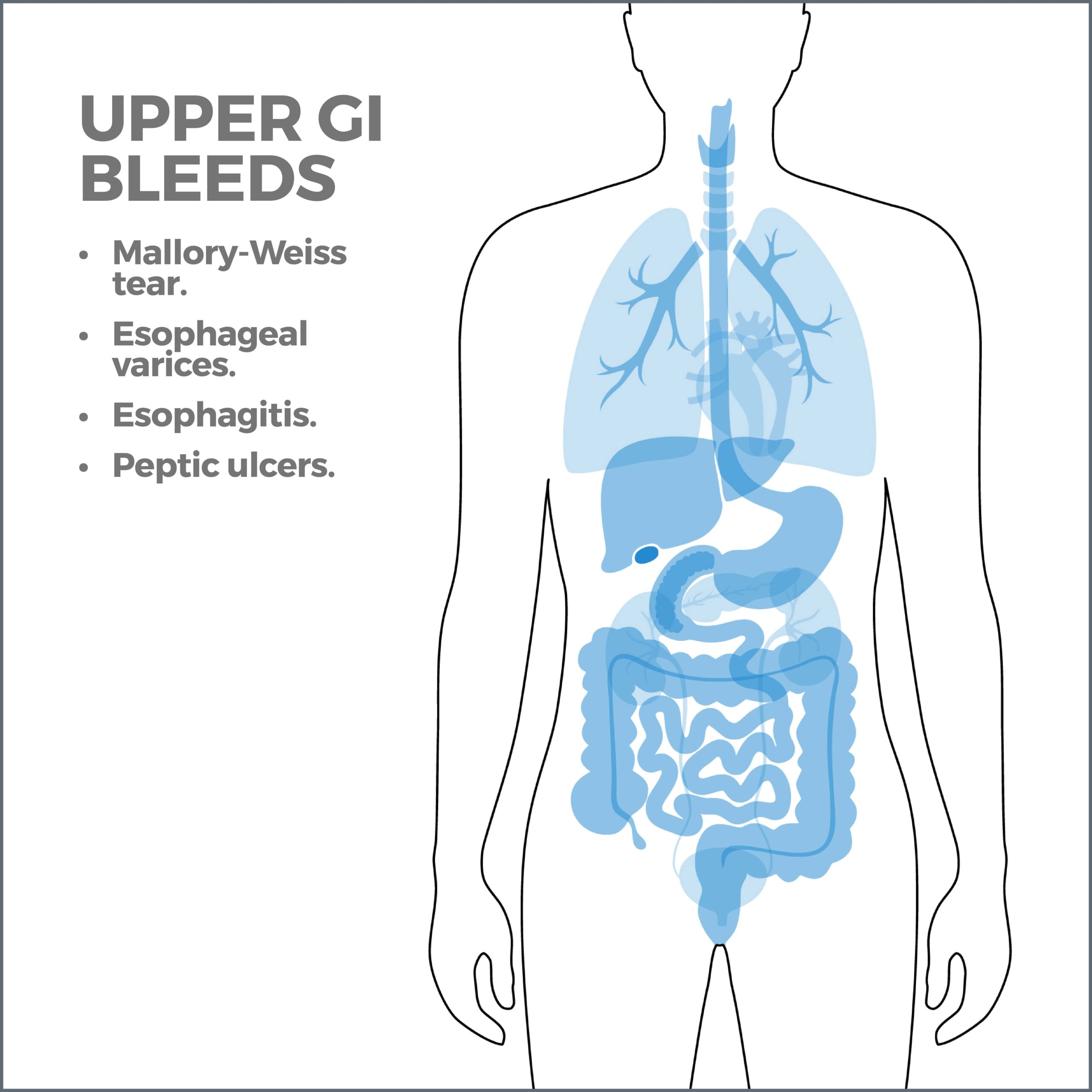
Upper GI Bleeds
Many problems with the GI tract can cause an upper gastrointestinal bleed, including:
Mallory-Weiss tear
A Mallory-Weiss tear is a fissure in the lower esophagus’ lining at or near the junction of the esophagus and stomach. It’s usually caused by intense retching or vomiting. It can also be triggered by things that increase abdominal pressure, such as hiccupping, coughing, epileptic seizures, CPR, childbirth, and heavy lifting. Mallory-Weiss’s tears typically heal on their own within a few hours. In rare instances, they can cause enough blood loss to require a transfusion.
Mallory-Weiss’s tears are most common in people between the ages of 40 to 60. Men are two to four times likelier to get them than women. Alcohol abuse is the leading risk factor for Mallory-Weiss’s tears. 50 to 75% of heavy drinkers get them.
Esophageal varices
Esophageal varices are abnormally large veins in the lower part of the esophagus or upper part of the stomach. If they break open and bleed, they can be life-threatening. Cirrhosis of the liver typically causes esophageal varices. More than 90% of people with cirrhosis are at risk for esophageal varices.
Most people are unaware that they have esophageal varices until the varices bleed. If the bleeding isn’t severe, you may swallow the blood, producing tarry, dark feces. You may vomit large amounts of blood when sudden and extreme bleeding occurs. If bleeding is uncontrolled, you may go into shock.
Esophagitis
Esophagitis is inflammation of the esophagus. It’s usually caused by gastroesophageal reflux disease (GERD). When you have GERD, the valve between your food pipe and your stomach malfunctions, and stomach acid backs up into your esophagus, causing a chemical burn. If this backwash happens often enough, it can irritate and inflame the esophagus until it bleeds. GERD can also be caused by eating disorders involving frequent vomiting, aspirin, infections, fungi, bacteria, allergies, drinking alcohol or coffee, obesity, and delayed stomach emptying.
Untreated esophagitis can have sever consequences. It may develop into Barrett’s esophagus, a condition that can elevate your risk for cancer or narrowing of the esophagus (esophageal stricture).
Peptic ulcers
Peptic ulcers are open sores on the stomach’s lining and upper section of the small intestine. They may bleed if they enlarge and eat away at a blood vessel. Peptic ulcers are typically caused by Helicobacter pylori bacteria or overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen. You may also increase your risk if you take blood thinners.
It’s a common misconception that spicy foods cause peptic ulcers. While they don’t cause ulcers, spicy foods, smoking, chewing tobacco, alcohol, and stress can aggravate ulcer symptoms.
Lower Gastrointestinal Tract Bleeds
Bleeding from the lower gastrointestinal tract is caused by conditions including:
Diverticulitis
Diverticula are small, bulging pouches in your large intestine’s wall. If these sacs become inflamed or infected, you have diverticulitis. Diverticula usually form when weak areas of your colon buckle under pressure. This force makes the diverticula bulge through the intestine’s lining. Low-fiber diets result in stools that don’t pass quickly, and straining during a bowel movement can cause diverticulitis.
Many people with diverticulitis don’t have symptoms, but others experience bloating, stomach cramps, pain on one side of the abdomen, or bleeding. When the pouches burst, the bleeding may be mild or severe. Most cases improve without treatment, although some cause severe blood loss and dehydration that need hospitalization.
Hemorrhoids
Hemorrhoids (piles) are enlarged veins inside the rectum (internal) or around the anus (external), like varicose veins. Internal hemorrhoids may bleed but are usually not painful. External hemorrhoids can hurt, itch, and bleed. Hemorrhoids can rupture, producing bright red rectal blood. The condition can resolve on its own with home remedies or over-the-counter treatments.
Hemorrhoids are mainly caused by straining to pass a bowel movement and a low-fiber diet. Piles are rarely dangerous. If your doctor suspects that the bleeding indicates a more serious gastrointestinal issue, they may perform a colonoscopy to diagnose the condition.
Ulcerative colitis
Ulcerative colitis is a long-lasting inflammatory bowel disease (IBD). It makes your immune system mistakenly attack your large intestine’s lining. This causes inflammation and open sores (ulcers). There is no cure; people usually have symptoms on and off their whole life. The main symptom of ulcerative colitis is bloody diarrhea. There may be pus in the feces, as well. If you have six or more bowel movements a day, you have a severe case of the disease.
Your risk for getting ulcerative colitis increases if you’re age 30 or younger, you’re of Ashkenazi Jewish descent, or a close relative has the condition. Ulcerative colitis can be treated with anti-inflammatory medications, immune system suppressors, or biologics. Your doctor may supplement these medications with anti-diarrheal treatments, pain relievers, iron supplements, or anti-spasmodic medications. Surgery involving colon and rectum removal may be necessary if other measures aren’t effective.
Colon Polyps
Colon polyps are small growths on your colon’s lining. You may have one or many. Usually, they’re harmless (benign), but some may become cancerous (malignant). Some take up to 10 years to become malignant. Anyone is susceptible to colon polyps, although the risk increases if you’re age 45 or older, are overweight, drink excessively, are sedentary, smoke, or eat a high-fat diet.
Colorectal cancer is the only cancer that’s almost 100% preventable. It’s crucial to get colonoscopies regularly. The procedure can locate and remove polyps in their early stages before they have a chance to become malignant. Most polyps don’t have symptoms, so a colonoscopy can detect them even if you don’t feel well. Symptoms may include bloody stools, anemia, weight loss, belly pain, diarrhea, or constipation lasting more than a week.
A healthy diet of fruits, vegetables, fish with omega-3 fatty acids, whole grains, and foods rich in vitamin D and calcium can lower your risk for colon polyps.
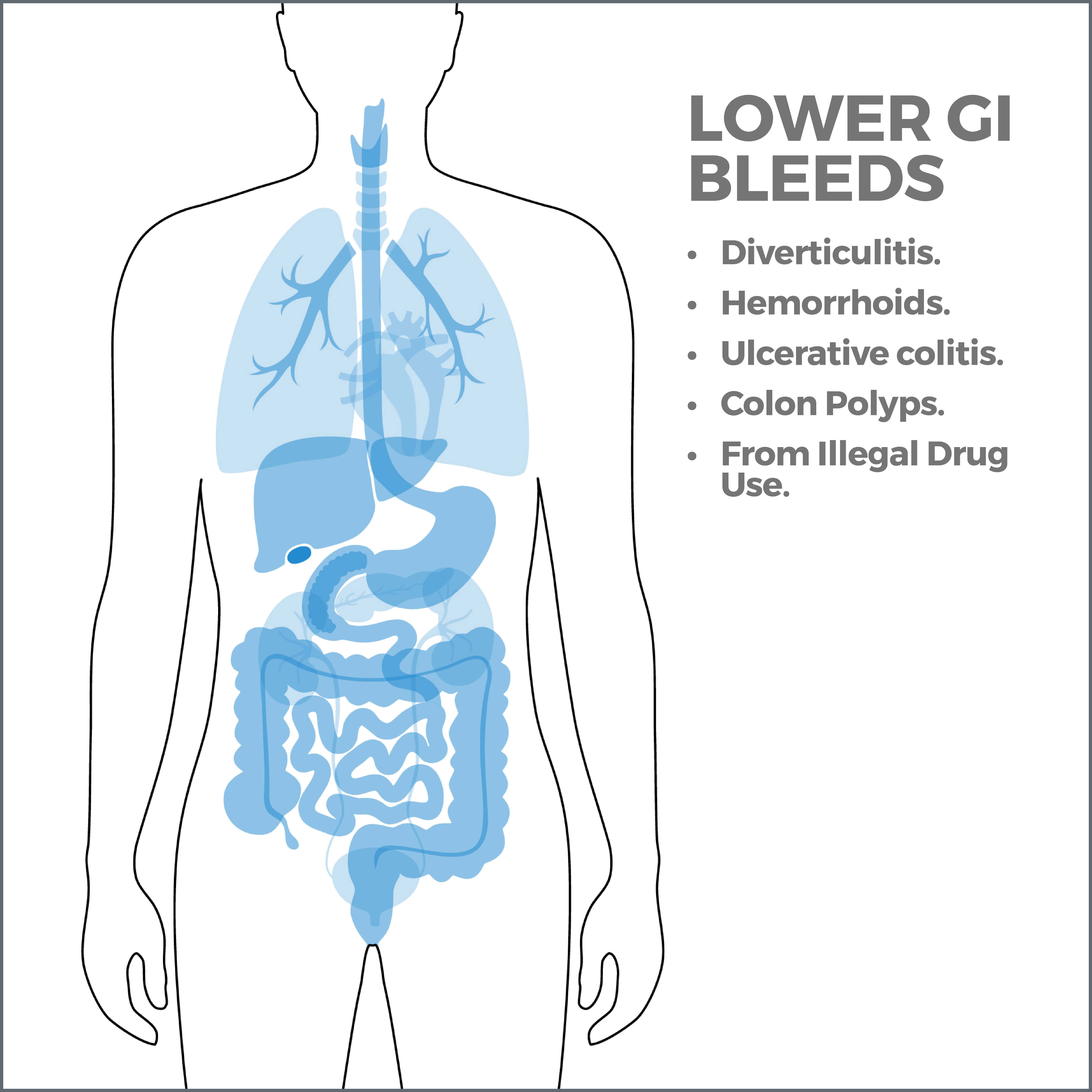
Gastrointestinal Bleeds from Illegal Drug Use
A study published in the American Journal of Forensic Medicine and Pathology documented the connection between lower gastrointestinal bleeding and cocaine use.
Shock
Shock may result if GI bleeding occurs suddenly and rapidly. Symptoms of shock include:
- Dizziness.
- Shortness of breath.
- Paleness.
- Rapid pulse.
- Inability to urinate.
- Drop in blood pressure.
- Unconsciousness.
Bleed treatments include:
- Intravenous medicines and fluids.
- Blood transfusion.
- Laparoscopy. This is a treatment in which a tiny camera and surgical equipment are passed through your digestive tract to determine the blood’s source and provide treatment.
- Gastric lavage. During this procedure, the stomach’s contents are drained.
GI Bleeding and Older Adults
Colorectal cancer and hemorrhoids are the leading causes of minor GI bleeding in people 65 or older. Diverticular disease, peptic ulcers, and angiodysplasia (breakdown of the colon’s blood vessels) are the leading causes of severe bleeding. About 35 – 45% of all acute upper gastrointestinal hemorrhages strike older adults. These patients have a low tolerance for a bleeding digestive tract, so diagnosis and treatment need to begin faster than in younger people.
Contact Us
Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform many diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority!



