
Bleeding in the Digestive Tract
Gastrointestinal (GI) bleeding is bleeding that occurs in your digestive tract. It can happen anywhere from your mouth to your anus. Bleeding that originates in your stomach, esophagus, or the first section of your small intestine is called upper GI bleeding. Lower GI bleeding refers to bleeding in the lower part of the small intestine, rectum, large intestine, or anus.
GI bleeding is a symptom of a condition rather than a condition itself. The amount of bleeding can range from minimal to life-threatening. The blood is often visible in your vomit or bowel movements, although it can be undetectable without using special instruments or tests. Treatment depends upon the intensity and location of the bleeding.
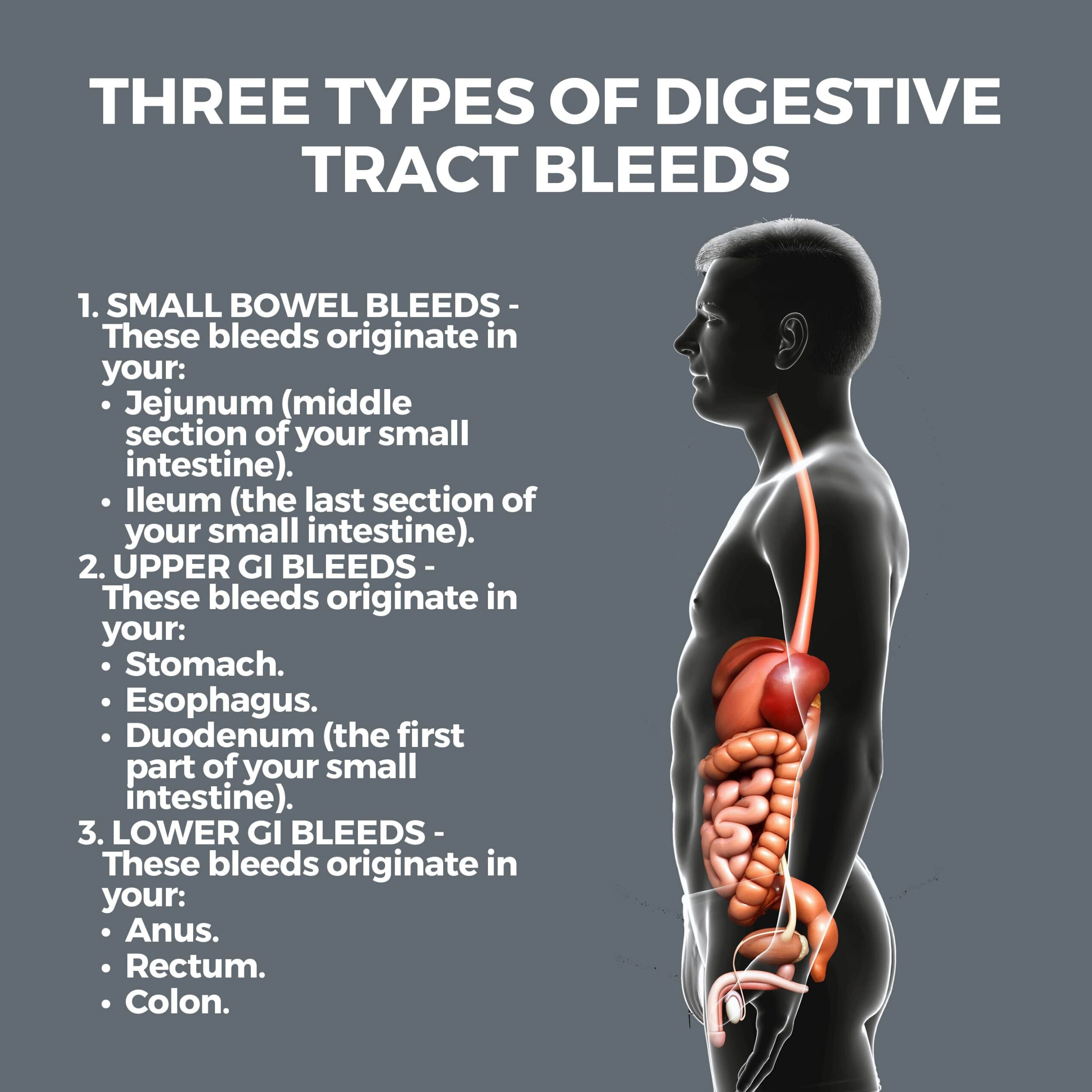
There are three types of digestive tract bleeds:
- Small Bowel Bleeds – These bleeds originate in your:
- Jejunum (middle section of your small intestine).
- Ileum (the last section of your small intestine).
- Upper GI Bleeds – These bleeds originate in your:
- Stomach.
- Esophagus.
- Duodenum (the first part of your small intestine).
- Lower GI Bleeds – These bleeds originate in your:
- Anus.
- Rectum.
- Colon.
When diagnosing GI bleeding, your doctor must first determine its source. Conditions that can cause it include:
- Angiodysplasia – When you have angiodysplasia, there are enlarged blood vessels in your GI tract. These blood vessels can weaken and bleed.
- Colon Polyps – Colon polyps are small growths on your colon (large intestine) lining that can cause bleeding. Some are benign, but some may be cancerous or become cancerous if not removed. It’s important to get a regular screening test called a colonoscopy – the gold standard of colon cancer detection. Colonoscopies have been shown to have 94% accuracy.
- Diverticular Disease – This condition causes gastrointestinal bleeding when small sacs develop and burst through weak areas of your colon’s wall.
- Esophageal Varices – Esophageal varices are enlarged, swollen veins in the esophagus. They could be life-threatening if they burst and bleed. This condition is related to serious liver disease.
- Esophagitis – Esophagitis causes stomach acid to back up into your throat. Throat tissue can bleed if eroded by this acid. If left untreated, you may need surgery.
- Hemorrhoids – Hemorrhoids are inflamed blood vessels around your anus or in your rectum. If you’re constipated or strained when passing a bowel movement, hemorrhoids can become painful, itchy, bulge, and sometimes bleed. Although they’re uncomfortable, hemorrhoids are not dangerous.
- Peptic Ulcer – Peptic ulcers are sores on your stomach’s lining typically caused by a bacterium called H. pylori or by prolonged use of nonsteroidal anti-inflammatory (NSAID) medications, including Aleve and Motrin. Peptic ulcers are not caused by spicy foods, a rich diet, or stress. The sores erode (perforate) the stomach’s lining and can cause bleeding. Blood loss can be slow and cause anemia, or extreme and require an immediate transfusion or hospitalization.
- Proctitis – Proctitis is an inflammation of the rectum’s lining and can cause bleeding. It is primarily related to unsafe sex, inflammatory bowel disease, and certain types of radiation therapy.
- Tears in the Esophagus – These are called Mallory-Weiss tears and can cause profuse bleeding. You can have more than one of these tears at a time. This condition primarily occurs in people who drink excessive amounts of alcohol.
- Ulcerative Colitis – Ulcerative colitis is an inflammatory bowel disease. It can cause bleeding in the digestive tract.
Types of Gastrointestinal Bleeding
There are five categories of gastrointestinal bleeding:
- Acute – This is severe, sudden bleeding that is a medical emergency.
- Chronic – Chronic bleeding is bleeding that comes and goes.
- Occult – Occult bleeding can’t be seen with the naked eye.
- Overt – In an overt GI bleed, blood is visible.
- Obscure – A GI bleed is considered obscure when a standard endoscopy doesn’t determine the bleeding’s source.
What Are the Symptoms of Gastrointestinal Bleeding?
These are several symptoms of GI bleeding. They may occur singly, or some may occur together:
- Bloody mucus.
- Dizziness or lightheadedness.
- Pale complexion.
- Shortness of breath.
- Weakness.
- Abdominal cramps.
- Fever.
- Anemia.
- Dehydration.
- Low blood pressure.
What Are the Symptoms of Acute GI Bleeding?
Acute GI bleeding is a medical emergency. If your bleeding starts suddenly and increases quickly, you could go into shock. Signs of shock include:
- Rapid pulse.
- Little or no urination.
- Unconsciousness.
- Drop in blood pressure.
If you have these symptoms, it’s imperative to call 911. You should also seek immediate medical care if you’re vomiting blood or have bloody, black, or tarry-looking stools.
If you’ve lost a lot of blood or continue bleeding, you might need intravenous fluids (IV), oxygen, or a blood transfusion.
The complications of a GI bleed include:
- Heart attack and other heart-related conditions.
- Cancer that advances without treatment.
- Infections.
How is Digestive Tract Bleeding Diagnosed?
Your doctor will diagnose the underlying cause of your bleeding by performing one or more of the following tests:
- Abdominal CT (Computerized Tomography) Scan – This test utilizes X-rays and a computer to create images of your GI tract.
- Blood Tests – A coagulation factor test may be performed to see how quickly your blood clots. It measures whether you have enough clotting proteins in your blood. When these protein levels are low, clotting can fail which triggers bleeding. You may also be given a blood test that assesses whether you have anemia.
- Capsule Endoscopy – You’ll swallow a vitamin-size capsule containing a tiny camera during a capsule endoscopy. As the camera travels through your digestive tract, it collects images your doctor can download and review. The capsule harmlessly exits your body during a bowel movement.
- Upper Endoscopy – During an upper endoscopy, a long, thin tube outfitted with a tiny camera is passed through your mouth and into your digestive tract to analyze your upper GI tract.
- Colonoscopy – A colonoscopy utilizes an instrument like the one used in an upper endoscopy, but it is used to examine your large intestine and rectum.
- Lower Balloon-Assisted Enteroscopy – During this test, a special scope examines areas of your small intestine that other endoscopic tests can’t reach. An endoscope with a deflated balloon attached is passed through your intestine. When the endoscope reaches an area that your doctor wants to examine, the balloon is inflated for a better view. An upper balloon-assisted enteroscopy can also be performed to view your stomach and upper digestive tract.
- Lower GI Test – This is an imaging test in which X-rays and a chalky substance called barium are used to view your large intestine. The same process can be used to view your upper GI tract.
- Nasogastric Lavage – During a nasogastric lavage, a tube is worked through your nose and into your stomach to extract its contents and analyze them for clues about the source of your bleeding.
- Stool Test – A stool analysis can help pinpoint the source of occult bleeding.
If these tests can’t locate the source of your bleeding, surgery may be necessary so that doctors can examine your whole small intestine, but this procedure is rarely used.
What Are the Risk Factors for Digestive Tract Bleeding?
- Smoking and drinking alcohol. Cigarettes and alcohol can increase your stomach acid.
- Overusing NSAIDs.
- A low-fiber diet.
- Excessive vomiting from an eating disorder.
- Taking anticoagulants. These medications, such as Warfarin, thin the blood and can increase the possibility of bleeding.
- Traumatic injury or recent surgery.
- Lack of screening for colon cancer.
- Older age.

Contact Us
Gastrointestinal bleeding can be quite alarming. The professionals at GastroMD are well-versed in determining the source of GI bleeding and devising a treatment plan.
Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in Tampa Bay. We perform a host of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority!



