
Indigestion
Indigestion is a broad term describing a group of digestive symptoms that can occur simultaneously. Also called dyspepsia or upset stomach, it’s a common condition that’s sometimes confused with heartburn, which occurs when stomach acid backs up into your esophagus. Although it could indicate a more serious, underlying disorder, indigestion is typically resolved by lifestyle and dietary changes.
What Causes Indigestion?
This condition occurs when you cannot digest food properly. It can be triggered by:
- Overeating.
- Eating too quickly.
- Foods that ferment in the gut. They include dairy products such as yogurt, asparagus, beans, lentils, cabbage, and processed foods. They contain probiotics, which are live microorganisms that bolster health and are generally digestible for most people. Some people react adversely to them and experience gas and bloating.
- Spicy, greasy, fatty, or fried foods.
- Foods containing excessive acid, including tomatoes, oranges, and grapefruits.
- Chocolate, carbonated beverages (including beer), alcohol, caffeine, and onions.
- Too many sugars and carbohydrates.
- Sugar substitutes.
- Chewing with your mouth open (swallowing too much air while eating).
- Lying down after eating.
- Having late-night snacks.
- Smoking.
- Fatigue.
- Stress.
- Overuse of alcohol.
- Wearing tight clothing: Tight clothing may squeeze your stomach and force acid into the esophagus. This includes belts, shapewear, and workout gear.
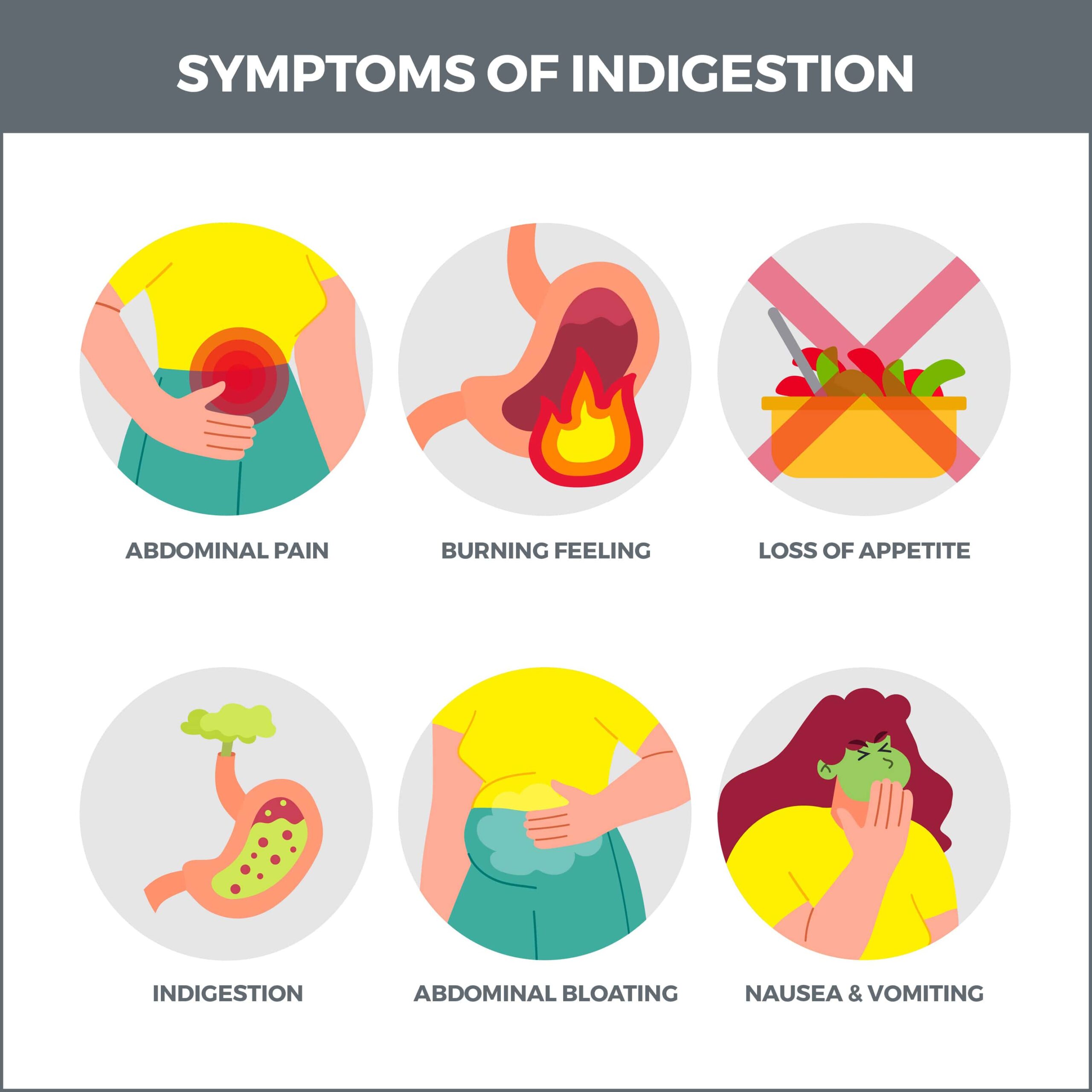
What Are the Symptoms of Indigestion?
The symptoms usually arise soon after you eat. They include:
- Feeling bloated: You have an uncomfortable feeling of tightness in your upper abdomen.
- Feeling full early during a meal: You haven’t eaten much yet, feel full, and may have trouble finishing your meal.
- Feeling uncomfortably full after a meal: You have a feeling of fullness long after eating.
- Abdominal pain.
- Nausea.
- Excessive belching or gas.
- Acidic taste in the mouth.
- Regurgitating.
- Stomach gurgling, with symptoms that get worse after you bend over or lie down.
There are three types of indigestion:
- Occasional: This type happens once in a while.
- Chronic: This type occurs regularly for weeks or months.
- Functional: When you have functional indigestion, you have chronic symptoms without a specific cause.
What Underlying Conditions Can Indigestion Indicate?
Sometimes, indigestion can point to a more serious, underlying condition such as:
- Hiatal hernia.
- Diabetes.
- Gallstones.
- Gastritis.
- Intestinal blockage.
- Gastroesophageal reflux disease (GERD).
- Gastroparesis (the stomach doesn’t get emptied correctly).
- Low amount of digestive enzymes.
- Reduced intestinal blood flow (intestinal ischemia).
- Irritable bowel syndrome (IBS).
- Stomach cancer.
- Thyroid disease.
- Pancreatic inflammation (pancreatitis).
- Stomach inflammation (gastritis).
- Peptic ulcer.
- Jaundice.
How is the Condition Diagnosed?
A physical exam is usually used as the initial evaluation if you’re not experiencing symptoms such as repeated vomiting and unexplained weight loss. But if you’re experiencing severe symptoms, your doctor may order:
- Stool and Urea Breath Tests: These tests check for Helicobacter pylori (H. pylori). This is a bacterium that is related to peptic ulcers.
- Laboratory Tests: Laboratory tests may detect metabolic disorders such as anemia.
- Imaging Tests (MRIs, CT scans, or x-rays): These tests may be done to discover intestinal obstruction.
- Endoscopy: An endoscopy may be done to check for upper digestive tract abnormalities. A tissue sample may be collected for evaluation. This test is particularly useful for analyzing older people with chronic symptoms.
How is Indigestion Treated?
Simple lifestyle changes may help to ease your condition. These include:
- Eating five or six small meals a day instead of three.
- Avoiding trigger foods, such as those listed above.
- Bypassing pain relievers such as aspirin, naproxen sodium (Aleve), and ibuprofen (Advil, Motrin), as well as steroids, thyroid medications, and certain antibiotics.
- Thoroughly chewing your food: Experts say you should chew soft foods 32 times before swallowing and 40 times for firmer foods. Since counting every chew could take the joy out of eating, aim for chewing food until it feels like a paste. (A good rule of thumb is if you can recognize food you’re eating from its texture, you haven’t chewed it enough.)
- Elevating your head and shoulders: This prevents stomach acid from traveling up your esophagus while sleeping. Do this by raising the head of your bed instead of using pillows, as this can harm your neck.
- Maintaining a healthy weight.
- Regularly exercising.
- Drinking plenty of water.
- Sitting straight while you’re eating.
- Staying hydrated: Hydration helps healthy digestion. It also helps flush out the acid that causes indigestion. This is most effective if you drink fluids after a meal, not while eating.
- Changing medications: Your doctor can help you change or stop medications that irritate your stomach. If this isn’t possible, take your meds with meals.
- H2 Receptor Blockers: H2 receptor blockers are medications that reduce acid that’s already in your stomach. H2 receptor blockers include Tagamet and Pepcid.
- Protein Pump Inhibitors (PPIs): Protein pump inhibitors block acid from being released into the stomach. They’re beneficial if you have heartburn as well as indigestion. PPIs include Nexium and Prilosec.
- Antibiotics: Antibiotics are helpful if H. pylori bacteria are responsible for your indigestion. They can also stave off infection by microorganisms such as salmonella, E. coli, and giardia. Antibiotics include amoxicillin and tetracycline.
- Prokinetics: Prokinetics means “to promote movement.” They can help your stomach empty faster. Prokinetics include Urecholine and Reglan.
- Antidepressants: When antidepressants are used for indigestion, it’s considered an “off-label” use. This means that they’re being used to treat something other than depression. They’ve been known to positively affect the contraction of the digestive tract muscles, sensitivity to abdominal pain, and the speed at which food travels through your digestive system.
Are There Other Treatments or Practices That Can Help?
Yes. Several other treatments and alternative practices have been successfully used in connection with indigestion. (Always check with your gastroenterologist for guidance before using.) These include:
- STW-5 (Iberogast): Also called “a blend of bitters,” STW-5 is a liquid containing nine herbal extracts, including dried peppermint leaf, dried angelica root, milk thistle, and lemon balm. It is best used for chronic conditions.
- Rikkunshito: Rikkunshito is a Japanese herbal blend containing herbs such as licorice root, ginseng, ginger root, and black atractylodes. It helps the stomach relax and empty its contents.
- Acupuncture: Acupuncture is a technique that utilizes fine needles inserted at specific parts of the body to relieve various ailments. For indigestion, these needles increase energy flow to the stomach to ease the condition.
- Yoga: Yoga can also be an effective means of managing stress. You can take classes if you prefer a group setting.
- Relaxation Exercises: For relaxation, you can try a body scan, breathing exercises, progressive muscle relaxation, or guided imagery.
- Meditation: Meditation can help you control the stress and tension that may be causing your condition. There are many forms of meditation, including mindfulness meditation, walking meditation, and sitting meditation, so you can choose the one best suited to you.
Will I Need Surgery?
If chronic acid reflux gives you ongoing indigestion, your doctor may recommend laparoscopic anti-reflux surgery (also called Nissen fundoplication). During this procedure, the valve between the esophagus and the stomach is reinforced by wrapping the uppermost part of the stomach around the lowest part of the esophagus.
What Are the Complications of Indigestion?
Usually, the problem is mild and only occurs occasionally. Severe indigestion can cause these complications:
- Pyloric Stenosis: Pyloric stenosis happens when the passageway between your stomach and small intestine (the pyloris) scars and narrows. This causes vomiting and improper digestion of food. Surgery can usually expand the pyloris to its correct width.
- Esophageal Stricture: When indigestion is caused by acid reflux, stomach acid flows back into the esophagus and irritates its lining. If this irritation continues, it can scar your esophagus. This scarring can eventually narrow and constrict the esophagus. This narrowing is known as a stricture. This condition can be remedied with esophageal dilation, a procedure that widens the constriction causing the narrowing. Strictures can cause:
- Chest pain.
- Food lodging in your throat.
- Difficulty swallowing.
- Barrett’s Esophagus: Barrett’s esophagus is a complication of gastroesophageal reflux (GERD). This is a chronic condition in which stomach acid backs up into your esophagus. When this happens frequently for many years, it damages the esophagus’ lining, triggering the formation of new, abnormal cells. The biggest concern about Barrett’s esophagus is that it’s a pre-cancerous disorder, although there is a small risk that it could develop into cancer.
When Should I Contact My Doctor?
Contact your gastroenterologist and get immediate medical attention if you have:
- Chest pain.
- Black stools.
- Bloody or frequent vomiting.
- Unexplained weight loss.
- Severe stomach pain.
- Jaundice.
- Difficulty breathing.

Contact Us
Contact us today! The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform various diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority!



