
Fecal Incontinence

Fecal incontinence (also called bowel incontinence) causes feces to accidentally leak from your rectum. This involuntary leakage may be minimal and occasionally happen when you pass gas or be a complete loss of bowel control. You may be aware or unaware that it’s happening.
Fecal incontinence is more common among women and older adults. Although the condition isn’t life-threatening, it can interfere with your quality of life, mental health, self-confidence, and sense of dignity.
How Do Normal Bowel Movements Work?
A bowel movement is made of leftover food that your body can’t digest. Several parts of the digestive tract are involved in defecating:
- Rectum.
- Anal Canal.
- Anal Sphincters.
- Hemorrhoids.
- Pelvic Floor.
The rectum is the end of the intestine. Feces collect here until the bowel is ready to be emptied. The anal canal is lined with nerves that alert you when your bowel is ready to be emptied.
Inner and outer sphincters are located at the end of the anal canal. A sphincter is a ring of muscle that relaxes or tightens to open or close a passageway in the body. The inner sphincter acts involuntarily. For example, it can prevent a stool from passing when you’re asleep. The outer sphincter can be deliberately controlled, so you can either hold or release a bowel movement.
Although hemorrhoids may be associated with inflammation, healthy ones help pass feces. Located at the end of the rectum, they’re cushiony sacs filled with blood vessels. Hemorrhoids and anal sphincters close the bowel to prevent stool from being released. The pelvic floor is a hammock-like group of muscles located in your pelvis. It relaxes to release feces and tightens to prevent them from being accidentally expelled.

How Do You Know That You Need to Pass a Bowel Movement?
As the rectum fills up with feces, nerve signals are sent to the brain, which processes them and sends them back to the anus. Then the pelvic floor relaxes, so the rectum’s muscles are alerted to push the stool out. You can follow this urge and voluntarily go to the bathroom or hold the feces in.
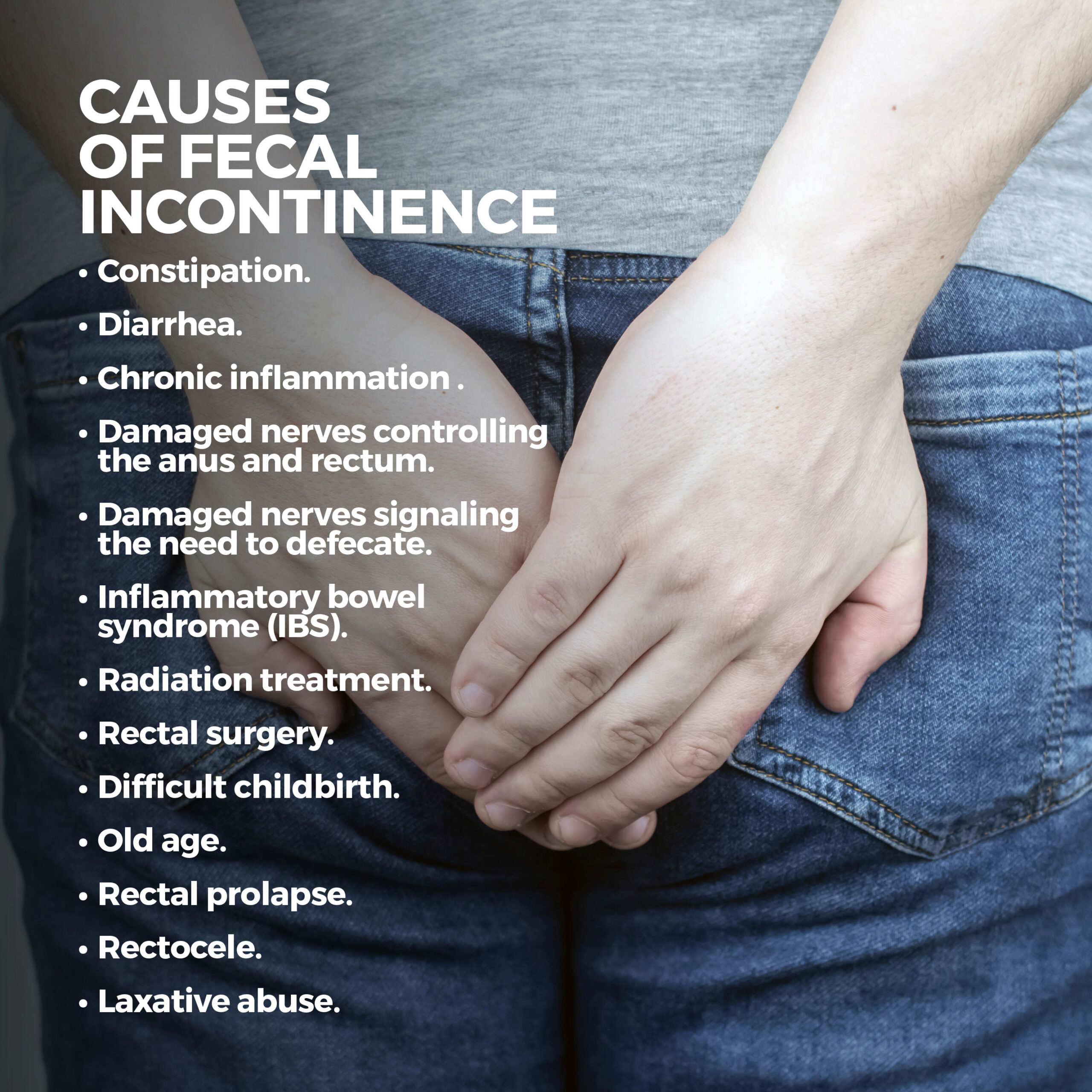
What Causes Fecal Incontinence?
Several things can cause fecal incontinence.
Constipation can produce big, hard bowel movements that are difficult to pass. Hard stools and persistent straining can weaken and stretch your rectum’s muscles. This makes it difficult to hold your feces. Feces leaking around a hard stool can also cause fecal continence. Diarrhea can worsen incontinence because it’s more difficult to hold in than a solid stool.
Chronic inflammation can stiffen the rectum, allowing feces to pass too quickly. You can also develop fecal incontinence if the nerves controlling the anus and rectum are damaged or the nerves signaling the need to defecate are damaged.
A healthy rectum stretches to hold feces until you defecate. But inflammatory bowel syndrome (IBS), radiation treatment, and rectal surgery can reduce the rectum’s elasticity. When the rectum can’t stretch enough to hold stool, it becomes incontinent.
Difficult childbirth can damage muscles that control bowel movements, especially if the doctor uses forceps or performs an episiotomy (a cut in the vagina to enlarge it during birth).
The following are additional causes:
- Old Age – Muscles in the anus and rectum and other parts of the pelvis weaken as you age.
- Rectal Prolapse – Rectal prolapse causes the rectum to fall into the anus.
- Rectocele – This condition develops when the rectum protrudes into the vagina.
- Laxative Abuse – Laxative abuse occurs when someone repeatedly uses laxatives to lose weight and reduce calories. This continuous use of laxatives can cause fecal incontinence.
What Tests Are Done to Diagnose Fecal Incontinence?
During a digital rectal exam, your doctor inserts a gloved, lubricated finger into your rectum to determine your sphincter muscles’ strength and detect abnormalities.
A balloon expulsion test involves inserting a small, water-filled balloon into your rectum. Next, you’ll go to the bathroom to try to expel the balloon. If you take longer than one to three minutes, it may indicate fecal incontinence.
Endoanal ultrasound is the gold standard for sphincter analysis related to fecal incontinence. Using sound waves, it produces images that your doctor uses to analyze your sphincter’s structure.
Anorectal manometry assesses various causes of fecal incontinence, especially inadequate anal sphincter tone. It can also identify impaired rectal reflexes and sensations.
During proctography, you sit on a specially designed toilet and have a bowel movement as x-ray images are taken. This test helps determine how well your body expels bowel movements and how much stool your rectum holds.
Pudendal Nerve Terminal Motor Latency tests determine whether your nerves can adequately control your anal sphincters. Your doctor will examine your rectum digitally with a miniature, finger-mounted electrode during this procedure. The electrode delivers a small shock to the pudendal nerve (which controls feeling in your sphincters). Your doctor will then measure the time it takes for the sphincter to contract when shocked.
Magnetic resonance imaging is a procedure that uses a powerful magnet and radio waves to create detailed, three-dimensional internal images.
How is Fecal Incontinence Treated?
Over-the-counter treatments are available to treat fecal incontinence:
- For diarrhea – Imodium (loperamide), Kaopectate, and Pepto-Bismol (bismuth subsalicylate).
- For constipation – bulk laxatives such as Citrucel (methylcellulose) and Metamucil (psyllium).
If you have fecal incontinence due to muscle damage, your doctor may suggest options that restore muscle strength and control. These include:
- Kegel Exercises – These exercises strengthen the pelvic floor muscles, which support the bowel. Kegels are done by squeezing the muscles you would use to stop urine flow. Like any exercise, the stronger you get, the more contractions you can do.
- Injectable Bulking Agents – Bulking agents (such as silicone, collagen, and hyaluronic acid) are injected into your anal sphincter to thicken it and impede leakage.
- Biofeedback – During biofeedback, sensors are strategically placed in the anus and rectum to train you to isolate and contract anal sphincter muscles.
- Radiofrequency Therapy – Also called the Secca procedure, radiofrequency energy is delivered to the anal canal, mildly injuring the sphincter muscles. As they heal, they become thicker and more resistant to leakage.
When is Surgery Necessary?
Surgery may be needed to correct an underlying issue causing fecal incontinence. This includes:
- Colostomy – A colostomy (or bowel diversion) involves rerouting stool through an opening in the abdomen. A bag attached to this opening collects the feces. A colostomy is only performed when other treatments have failed.
- Surgical Correction of Rectal Prolapse – This procedure reduces or eliminates fecal incontinence. The longer the prolapse goes untreated, the more the sphincter’s muscles and nerves will be damaged. This raises the risk that fecal incontinence will not improve after surgery.
- Sphincteroplasty – Sphincteroplasty addresses anal sphincters weakened or damaged during childbirth.
There are home remedies and lifestyle changes that can help you manage fecal incontinence:
- Eat Fiber-Rich Foods – If you have constipation, fiber softens feces so that they are more controllable. If you have diarrhea, fiber makes stools bulkier and less watery. You can get fiber from vegetables, fruits, whole-grain foods, and supplements.
- Eat Smaller, More Frequent Meals – Large meals can trigger bowel contractions that produce diarrhea. It’s okay to eat the same amount a day, but just break it down into several smaller meals. Sometimes large meals can cause diarrhea or trigger frequent bowel movements.
- Monitor What You Eat – For several days, keep a journal of the food you eat. You may see a connection between specific foods and your incontinence symptoms. Remove these foods from your diet and see if your condition improves. Common triggers include spicy, fatty, or greasy foods, cured meat, alcohol, and dairy.
- Cut Caffeine – Caffeine can overstimulate your bowels and cause diarrhea. Caffeine is a well-known ingredient in coffee and tea, but did you know it’s also in chocolate, sodas, some brands of chewing gum, and some over-the-counter pain relievers?
- Avoid Sweeteners – Steer clear of sweeteners such as xylitol, stevia, sorbitol, fructose, and mannitol, which can trigger diarrhea.
- Drink Plenty of Water – If you have constipation, staying hydrated will make your stools softer and more formed, making them easier to pass. Aim for eight eight-ounce glasses a day.
Contact Us
You may be hesitant to seek help for your fecal incontinence because you’re embarrassed about discussing it. At GastroMD, we understand your discomfort and will provide the utmost discretion as we discuss your personalized treatment plan.
Contact us today. The team of professionals at GastroMD looks forward to working with you. We are one of the leading gastroenterology practices in the Tampa Bay area. We perform a wide range of diagnostic procedures using state-of-the-art equipment in a friendly, comfortable, and inviting atmosphere where patient care is always a top priority.



